This is a cross-sectional observational study. Children's weight, height, blood pressure, serum levels of total cholesterol, triglycerides, HDL cholesterol, LDL cholesterol and non-HDL cholesterol were objectively measured from participants. Statistical analysis was performed using the ANOVA technique for parametric data and the Kruskal-Wallis test for nonparametric data. Study was conducted on 157 children aged 7-9 from two educational institutions located in low-income areas in Bogotá, Colombia. Weight excess (overweight and obesity) was observed in 46 subjects, of which 97.8% had a high or very high waist circumference. The lipid profile was altered in 45.2% of the subjects; 22.3% presented high levels of triglycerides. Metabolic syndrome was identified in 32.6% of the subjects with excess weight, thus being the most frequent component of high or very high waist circumference. Finally this study confirmed the high prevalence of malnutrition by excess weightand, also excess weight associated with high triglyceride and low HDL levels. The results of this study suggest the need for early and thorough interventions aimed at improving the lifestyles and quality of life of children.
Key words: Cardiovascular risk, metabolic syndrome, dyslipidemia, children, overweight, obesity, childhood hypertension.
Este es un estudio observacional transversal. Se realizó valoración antropométrica, bioquímica y de presión arterial en 157 niños y niñas con edades de 7 a 9 años de dos instituciones educativas, localizadas en sectores con recursos económicos limitados de Bogotá. Se determinó niveles séricos de colesterol total, triglicéridos, colesterol HDL, colesterol LDL y colesterol no-HDL. Se realizó análisis estadístico mediante la técnica de ANOVA para datos paramétricos y la prueba de Kruskal-Wallis para datos no paramétricos. Se observó exceso de peso (sobrepeso y obesidad) en 46 sujetos de los cuales el 97.8 % presentó circunferencia de cintura alta. El perfil lipídico se encontró alterado en el 45.2 % de los sujetos; el 22.3% presentaron triglicéridos elevados. El síndrome metabólico se identificó en el 32,6% de los sujetos con exceso de peso, siendo el componente más frecuente la circunferencia de cintura alta. En este estudio se pudo confirmar la alta prevalencia de malnutrición por exceso y también el exceso de peso asociado a valores altos de triglicéridos y niveles bajo de HDL. Este estudio sugiere la necesidad de intervenciones tempranas e integrales enfocadas a mejorar los estilos y calidad de vida de los niños y niñas.
Palabras clave: Riesgo cardiovascular, síndrome metabólico, dislipidemia, niños, sobrepeso, obesidad, hipertensión infantil.
Lipids and Diabetes Division, Department of Physiological Sciences, National University of Colombia. Bogotá, Colombia
In recent years there has been an increasing number of cases associated with cardiovascular disease (CVD) that, according to the World Health Organization (WHO), are the leading cause of death worldwide.Several studies have shown that the prevalence of overweight (OW) and obesity (OB) in children has also increased, which is a cause for concern, not only for its short-term consequences, but also for their health condition in adulthood (1, 2) as it is closely linked to the subsequent development of cardiovascular disease, increasing the risk of mortality at a young age. In a study of children and adolescents in Bogalusa, the connection between body mass index (BMI) and the accumulation of fat and atherosclerotic plaques in coronary arteries has been proved; a strong link between cardiovascular risk factors and BMI was also discovered showing a positive relationship with the levels of total cholesterol (total-c), LDL cholesterol (LDL-c), very low density lipoproteins (VLDL) and arterial pressure (AP) (1).
In Colombia, child obesity and overweight have increased (every 6th infant between 5 and 17 years presents OW or OB)(3), which have been corroborated in studies of schools in Bogotá(4). Part of the explanation for this phenomenon is the increase in sedentary lifestyle. The 2010 Encuesta Nacional de la Situación Nutricional de Colombia (ENSIN – National Survey of the Nutritional Situation in Colombia) reports that 57.9% of children aged 5 to 12 watch TV or play video games 2.4 hours or more a day, and adolescents 2.8 hours per day (3).
Several studies have shown that the most important factors in the appearance of OW and child OB are inadequate eating habits and physical inactivity (5); these factors also affect the level of circulating lipids;has been observed, in other studies, a significant relationship between cholesterol and lipoproteins in childhood to adulthood(6).
Dyslipidemia and OB are the result of multiple causative factors that, among others things, include: genetic; environmental and socio-cultural factors; eating habits; lifestyle; and physical activity(7). It is necessary to study the behavior of these variables to increase knowledge of this problem in the population and contribute to the implementation of contextualized strategies (5).
Another measurement that has become important because of its relationship with cardiovascular risk is waist circumference (WC), which is an indicator of the amount of visceral adipose tissue. Several studies have reported that this circumference is correlated with a family history of diabetes, high levels of LDL-c, low HDL cholesterol (HDL-c) and high AP (5). Measuring waist circumference is important, because the abdominal adiposity is a predictor of CVD and type 2 diabetes, even independently of BMI(6).
FA cross-sectional observational study was conducted to identify levels of cardiovascular risk factors and nutritional status of children aged 7-9 in two educational institutions in the city of Bogotá during the second semester of 2014. The study was approved by the Ethics Committee of the Faculty of Medicine at the National University of Colombia.
The population consisted of all students between 7 to 9 years 11 months, enrolled in educational institutions in February 2014, with 230 subjects of Llano Oriental School (IED Llano Oriental) and 142 of Liceo Integral Los Alisos. Of the two institutions 185 subjects complied with the inclusion criteria and provided their informed consent (according to the current regulations for human subject research, resolution 08430/1993 of the Ministerio de Salud de Colombia); 3 boys and 4 girls were not present at the time of the assessments, so 178 children were included in the study. Given the amount of time that had passed since providing consent, 21 children were 10 years old at the time of the nutritional assessments, and therefore were not included in the statistical analysis. Thus, the final study group was composed of 157 subjects (70 boys and 87 girls).
Anthropometry: Weight was measured on a precision digital scale (Tanita), the participants were barefoot and wearing light clothing. Height was measured with stadiometer (SECA) applying the techniques according the Manual of techniques for anthropometric measurements to health professionals. According to the instructions for the implementation of the growth patterns of WHO in Colombia for children and adolescents of 0-18 years (8).
Nutritional interpretation was performed according to The WHO Child Growth Standards for children of 5-18 years(8).
The Waist Circumference (WC) was measured in the horizontal plane at the midpoint between the last right rib and the iliac crest using an inelastic fiberglass tape (OMS). Values of CDC was used to assess high/waist circumference(9).
Blood samples were taken from the antecubital vein after 12 hours of fasting. To determine the lipid profile and blood glucose levels, samples were set in the centrifuge at 3500 xg for 5 minutes and the serum obtained was stored at -20 °C. Enzymatic spectrophotometric techniques were used to determine total-c, triglycerides (TG), HDL-c and glucose; LDL-c was calculated using the Friedewald equation and non-HDL cholesterol (non-HDL-c) by the difference in total-c – HDL-c. A classification of the risk of fractions of the lipid profile was undertaken according to the NHLBI guide for screening and cholesterol cutoffs, referencing the study of The National Cholesterol Education Program, which also considers the levels of c-non-HDL (10).
Although the Metabolic Syndrome (MS) should not be diagnosed in children under 10 years (Diabetes Federation (11)) we want to identify the possible cardiovascular risk associated with metabolic syndrome in children in this study. Cook's parameters were used as reference to identify alterations of metabolic syndrome (Cook et al (12)) (WC ≥ p90, systolic and / or diastolic ≥ 90 Pc for age, TG ≥ 110 mg / dL, HDL ≤ 40 mg / dL or fasting blood glucose levels ≥ 100 mg / dL).
The Blood Pressure (BP) was obtained using an aneroid sphygmomanometer with a cuff appropriate for the arm circumference and age of the participant (Starmed CE 0123). The measurements of were performed in duplicate, and the mean of the 2 readings was used as the final measure. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents study was used to assess BP in children considering gender, age and height (13).
The subjects were classified into six groups according to BMI, height and waist circumference. The groups were: 1) risk of thinness, 2) adequate weight, 3) overweight, 4) obesity 5) risk of stunting or low height and 6) high or very high waist circumference without being overweight or obese according to BMI. The database was processed using the R2012a program MATLAB (7.14.0.739) Mathworks for the analysis of the anthropometric variables and lipid profile. The Shapiro-Wilk test was used to determine normality, and Levene's test for homogeneity of data.
The ANOVA technique (analysis of variance) was used to compare parametric data (for normality and homogeneity) and the Kruskal-Wallis test was used for nonparametric data. Numerical variables were expressed as mean, standard deviation and percentages.
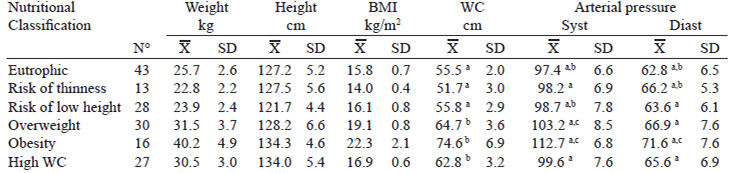
Anthropometric data and biochemical variables of the studied population are shown in Table 1.
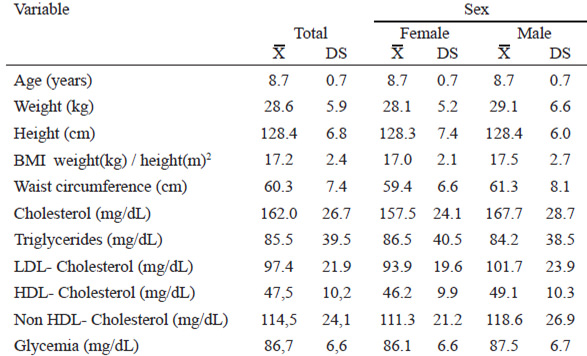
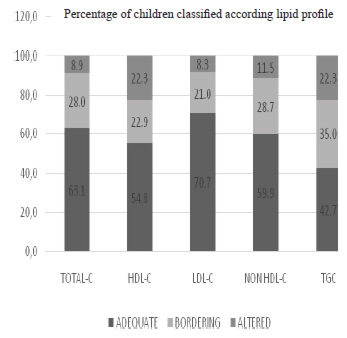
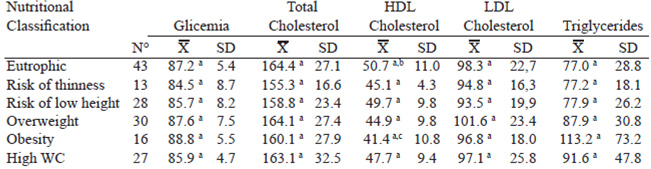
19.1% of children were within desirable limits for lipid profile variables (Table 1), though it was evident that the majority of participants (45.2%) had elevated levels of some variable lipid profile and alarm levels (bordering on 37.5%) according to level limits recommended by the NHLBI (Figure 1). There were no cases of c-LDL higher than 160 mg /dL. All children had blood glucose levels within reference values (Table 4).
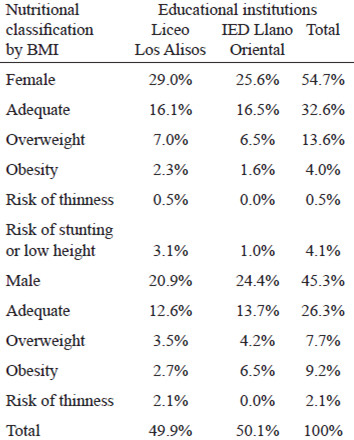
Further, the study showed that 46 children (29, 3%) presented weight excess (OW and OB) (Table 2), of which 97.8% had high or very high WC (greater than the 75th percentile); only one OW participant presented adequate WC. The groups of subjects with OW and OB had a WC significantly higher than eutrophic children and children with risk of thinness (p <0.01). 19.1% of subjects with adequate weight presented high WC.
In addition, 56.5% of children with weight excess presented at least one altered variable in the lipid profile and 26.1% were found in the border range of any other variable, indicating that 82.6% of children with weight excess have cardiovascular risk. Nonsignificant differences between the groups were found in values of total-C, TG, LDL-C and non-HDL-c, but a significant difference in the levels of HDL-c between groups of subjects with OB and healthy children (p <0.05) was seen (Table 4).
It was observed that the prevalence of high diastolic and systolic pressure values in subjects with OW was 8.6 and 5.7 times more than in eutrophic children, respectively. In OB, the probability of elevated systolic blood pressure (SBP) and diastolic blood pressure (DBP) was 18.8 and 9.4 times respectively compared to eutrophic subjects. Table 3 shows the significant difference found in DBP and SBP among subjects with OB and eutrophic, as well as the SBP in children with OW vs. eutrophic.
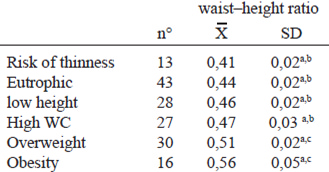
The waist to height ratio ((WHtR) was calculated as a parameter predictor of cardiovascular risk reported by other authors calculated in children and adults (14, 15). The results for the different groups are found in Table 5.
Diagnosis of metabolic syndrome was made with insulin resistance and abdominal obesity as the main components. At least three altered criteria were taken into account, a prevalence of metabolic syndrome in 32.6% was found in OW and OB children (15 subjects).
In this study, a high prevalence of OW and OB was found in a school children population from disadvantaged socio-economic classes. As for other research in Colombia, similar results were found in a study conducted by Fajardo in Bogotá (4)where 22.4% of OW and 15.3% of OB in children 7-11 years of age were reported. In turn, Uscátegui in Medellin (2) found that only 9.3% of children were OW and 4.6% OB, which may reflect cultural differences associated with nutritional status in different regions of the country. This high prevalence suggests that weight excess is a public health problem resulting from various factors such as the current food insecurity in disadvantaged socioeconomic classes of countries with intermediate economies, which have increased risk of OB as opposed to the high economic stratum (16).
The OB has generated an increasingly frequent occurrence of noncommunicable diseases related to nutrition, which in turn generate additional health costs for treatment and its consequences (16). Although clinical manifestations of CVD usually do not make their appearance until middle age, the atherosclerotic process begins at the earliest stages of life and altered lipoprotein levels are associated with atherosclerosis in youth. In assessing the lipid profile of children, serum alterations of TG, non-HDL-c and HDL-c are found, suggesting an increased risk for these children to develop CVD, with similar results to those described by Rosillo in Argentina (17) and Uscátegui in Medellin (2) The percentage of children with high TG in our study was higher than reported in Mexico (18), but lower than described in Argentina and Venezuela (17, 19), which is possibly due to different environmental and cultural conditions that influence the development of CVD.
The concentrations of LDL-c in our study were higher than those reported by Marcano (20)and similar to Leeson et al. (21), who found an inverse relationship between serum cholesterol levels and lower distensibility of the brachial artery in 9-11 years-old children. Regarding to HDL-c in this study, the total number of children with low HDL-c was 28.7% but it is worth noting that 11.5% were found to have levels between 40-45 mg/dL, which is considered borderline according to the breakpoints of the NHLBI. The percentage of patients with low HDL-C levels in our population is lower than those reported in other studies in Latin America (18, 20) even though they use the same breakpoint (<40 mg/dL). This difference could be explained by different lifestyles such as eating behaviors and physical inactivity (22).
In this study a higher frequency of elevated levels of c-no-HDL vs. LDL-C was found. The determination of non-HDL-c, was proposed by Bamba (23) as a detection tool for cardiovascular risk. The non-HDL-c can permit a timely intervention to identify children with components of MS or who are at risk; it can also be used to predict the severity of atherosclerosis and CVD in adults.
BSP and BDP prevalence were higher in this study in comparison with other research conducted in Mexico and Argentina (24, 25). The relationship between HBP (High blood pressure) and exogenous obesity is well known (26). Dei-Cas et al. found that 4.7% of female and 13% of male adolescents were hypertensive, of which 7% were OB. Both BSP and BDP were correlated with BMI and OW (27). A similar situation was observed in this study about the positive relationship between weight excess (OW and OB) and high BSP and BDP levels, independently or combined. Lozada (19) also reported a statistically significant association between OB, hypertriglyceridemia and BP. Weight excess is strongly linked to HBP (24, 26). In this study the possibility of high SBP with OW increased 8.6 times, and the DBP was 5.7 times higher in comparison to children with normal weight; in the case of OB, the possibility of high SBP increases 18.8 times and for high DBP increases 9.4 times in comparison to eutrophic children, reflecting similar data found in a Mexican study (28).
The waist-to-height ratio (WHtR) has been considered by several studies as a good indicator of central adiposity which evaluates cardiovascular risk in adults and children (14), it is quick and easy to calculate in daily practice (29). Some authors have proposed a WHtR > 0.5, which would have a high predictive capacity of higher cardiovascular risk (15, 30). In this study we were able to identify the WHtR was statistically higher in children with OW and OB (> 0.5), which is considered a good predictor of cardiovascular risk, taking into account that these children had a higher number of alterations in blood pressure and lipid profile. Our results are consistent with those we found in other studies in child population, like Rangel et al. (14) who noticed a relationship between WHtR on the development of high blood pressure or hypertension in Mexican children. Also studies in the UK and Chile (15, 30, 31) demonstrated the relationship between the OW and obesity with an indicator> 0.5. WHtR has been reported as a better predictor of cardiovascular risk compared with waist-hip ratio and the BMI (14, 31, 32).
32.6% of children with weight excess in this study presented alterations associated to MS, which is higher than the percentages found in studies conducted in Venezuela (19)and Mexico (33) in older children.
In this study, the main alterations were identified: waist circumference values above the 90th percentile, low levels of HDL-c, and elevated TG. This agrees with the findings of Burrows et al. who demonstrated that in a population of children with MS the most common risk factor was abdominal obesity (76%), followed by hypertriglyceridemia (39%) and hyperglycemia (4%) (34). In recent years, an increase in the diagnosis of MS has been observed, which could be attributed not only to the interest in detection, but also to the changes in lifestyle at an early age. Increase of MS in childhood leads to an increased frequency of noncommunicable diseases and worsens the prognosis of these diseases in adulthood. Early detection of MS components may then have a positive impact on the health of children and adults.
Dyslipidemia in children is a real problem, as during the study significant elevations of TG were observed as well as a decrease in HDL-C, which increases the risk of cardiovascular disease and leads to the premature development of MS.
Knowledge of the risk factors of CVD in children is very useful because it allows for prevention initiatives at an early age, which in turn reduces the incidence of cardiovascular disease in the future.
It has been suggested that the waist to height ratio (WHtR) above 5 can detect early cardiovascular risk factors, this was evidenced in overweight and obesity children.
The authors wish to thank the students and the academic and administrative staff of educational institutions IED Llano Oriental and Integral Liceo los Alisos for their great help and support in the project.
Recibido: 04-07-2015
Aceptado: 19-10-2015