Adolescents’ eating habits are determined by social, psychological, economic, political, and educational influences. They tend to prefer foods with inadequate nutritional value and high fat and carbohydrate content which leads to excessive weight gain and for many, calcium intake is restricted. According to some authors, low calcium intake is linked to increased adiposity. The objective was to evaluate adolescent calcium intake and investigate a possible relationship between calcium intake and nutritional state. As part of their first consultation at Botucatu Adolescent Outpatient Clinic – UNESP, 107 adolescents were nutritionally classified by BMI, according to age, gender, and bands proposed by CDC and AAP. Diet was evaluated by a 3 day 24h food recall, adopting 1300mg/day calcium intake as recommended by Dietary Reference Intakes. Median calcium intake for the whole sample was 546.6mg/day, with 91.30% female and 86.84% male presenting lower than adequate daily recommended ingestion levels (DRI). There was significant difference between calcium densities (Ca mg/1000kcal) in eutrophic and overweight/obesity in males. Male adolescents showed an inverse relationship between calcium intake and adiposity (r= -0.488 and p=0.0173), which corroborates the hypothesis that low calcium intake is linked to fatty tissue gain. Only 8.70% of female and 13.16% of male adolescents reached their daily recommended calcium intake levels. It must therefore be stressed that nutritional education is an important protection factor for children and adolescents in later life.
Key words: Adolescence, obesity, calcium intake, bone health.
Los hábitos alimentarios se desarrollan dependiendo de los determinantes sociales, psicológicos, económicos, políticos y educacionales y sus preferencias recaen sobre alimentos con inadecuado valor nutricional, elevado contenido de grasa y carbohidratos que conducen a un aumento excesivo de peso. De acuerdo con algunos autores la baja ingestión de calcio se asocia al incremento de la adiposidad. Los objetivos fueron evaluar la ingestión de calcio por adolescentes e investigar una posible relación con el estado nutricional. En su primera consulta en el Ambulatorio de Medicina del Adolescente-Botucatu-UNESP, 107 adolescentes se clasificaron nutricionalmente por el IMC, de acuerdo con la edad y sexo y puntos de corte propuestos por el CDC y AAP. La evaluación dietética fue realizada por el método de recordatorio de 24 hrs. en 3 días diferentes y se adoptó la recomendación de Dietary Reference Intakes (DRI), de 1.300 mg de Ca/día. La ingestión mediana de calcio para la muestra total fue de 546,6 mg/día. Un 91,3% de las adolescentes y un 86,8 % de los jóvenes presentaron un consumo inferior a los valores de DRI. Al comparar la densidad de calcio (Ca mg/1.000 kcal) entre los grupos eutróficos y sobrepeso/obeso del sexo masculino, se constató una diferencia significativa. En los adolescentes masculinos se evidenció una relación inversa enttre consumo de calcio y adiposidad (r = -0,488 y p = 0,0173), lo cual confirma la hipótesis de que la baja ingestión de calcio se asocia al aumento de tejido graso. Solamente el 8,7% de las adolescentes mujeres alcanzaron las recomendaciones diarias de DRI y de los adolescente masculinos, el 13,16%.
Palabras clave: Adolescencia, obesidad, ingestión de calcio, salud ósea.
Botucatu School of Medicine, São Paulo State University (UNESP), São Paulo, Brazil.
Financial support by FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo) Process No 04/07007-1.
Adolescence, according to The World Health Organization (WHO) is from 10 to 20 years of age. The Brazilian Health Ministry defines adolescence as the same aged subgroup of the population as WHO, considering it as the period of life with intense growth and development, and anatomical, physiological, psychological, emotional and social transformation (1). On top of these, adolescence is also the critical time of life where life habits, among those dietary, are established (2,3).
Food consumption in this stage of life is influenced by many factors; these include: sociocultural values, gaining a new body image, getting on with peer groups, family financial situation, providing or not providing food acquisition, food eaten outside the home, consumption of processed foods, the media, acquiring food habits reflected in choice, monotony, and way of preparing them (4,5).
Scientific literature highlights that adolescents diets are characterized by their preference for high energy foods, containing high levels of saturated fats and cholesterol as well as large quantities of salt and carbohydrates, with reduced nutritional value, resulting in not attaining the minimum recommendations for different groups of foods (2,6).
These changes in eating habits, lifestyle, and social behavior may be responsible for the significant increase in non-transmittable chronic diseases such as: osteopenia and osteoporosis, overweight and obesity and their side effects, arterial hypertension, dyslipidemia, type 2 diabetes mellitus, insulin resistance syndrome (IRS) which can affect them in adolescence or when they reach adulthood (7,8). It is also important to know food consumption as different studies have shown correlation between diet composition and the risk of morbimortality (2,7,8). In relation to the above dysfunctions, calcium metabolism has received more international attention (9,10), especially in relation to osteoporosis (11-13), arterial hypertension (7) and in weight control (14-17).
Specifically in relation to obesity, a lot of effort has been focused on understanding total energy balance and diet macronutrient levels, however few studies have looked at the role of macronutrients have on energy balance (18). In this context, dietary calcium has been recognized as a mineral which boosts weight loss (18,19). Metabolically, the probable mechanism is that a reduction in dietary calcium intake increases intracellular calcium due to changes in parathyroid hormone and 1,25 dihydroxyvitamine D levels. Increased intracellular calcium in adipocytes, potentializes lipogenesis and inhibits the lipolitic process (9). With this in mind, researchers have suggested that adequate calcium uptake increases body fat oxidation rates (20), however the exact mechanisms are still not fully understood and lead to controversy between studies (18,21).
The daily recommended consumption level of calcium for 9 to 18-year-olds of both sexes is 1300mg per day (DRI, Institute of Medicine 1997) (22). However it needs to be considered that there are still barriers to consuming foods high in calcium; these include palatability, inconvenience, possible calorie content and digestive complications, on top of insufficient knowledge about its metabolic value (11,12).
In light of considerations which emphasize the increased prevalence of obesity in adolescents, changes in their eating habits, and their reduced calcium intake, the objective of this study was to nutritionally evaluate adolescents attending outpatient clinics for this age group, determine levels of eutrophy, overweight, and obesity; understand their food consumption, focusing on calcium intake and the possible relationships between low calcium intake and the prevalence of overweight and obesity in individuals.
One hundred and seven adolescents in the 10 to 19 years old age bracket were evaluated at Botucatu School of Medicine Adolescent Outpatient Clinic from August 2003 to December 2004, after approval from the Research Ethics Committee of Botucatu School of Medicine - UNESP OF.51/2004-CEP.
Adolescents and their parents or guardians were made fully aware of the content through explanations given at the outpatient clinic and were included in the study after receiving and returning the free informed consent forms signed by both the adolescent and their parent or guardian. Non-adhesion to the study did not imply any sanction whatsoever for the adolescent, who was evaluated as per all procedures performed in this outpatient clinic.
Exclusion criteria were adolescents submitted to prolonged corticoid treatment or who used calcium supplements, those with the following ailments: diabetes mellitus, chronic or acute malnutrition, congenital or acquired bone diseases, gastrointestinal disorders accompanied by poor absorption, history of nephropathy, with or without chronic renal insufficiency, endocrinopathies, early or late puberty, chronic drug consumption, those considered as return patients as they had already received nutritional guidance in previous consultations, which could have interfered in their dietary evaluation.
Socioeconomic evaluation was performed to identify the population standard using a questionnaire developed by the National Association of Research Companies (ANEP), which considered head of family schooling level, and material goods in the home (23).
All adolescents who made their first consultation during this period, considered new cases in this clinic, underwent anamnesis and full clinical and anthropometric and nutritional examinations. However, the final sample was composed of those not satisfying any of the exclusion criteria. They were weighed on electronic platform 150kg capacity 100g graduation scales (Filizola), with minimum clothing (100g) and barefoot (24).
A wall mounted height gauge with mm scale was used for measuring stature according to Jelliffe, considering the average of two measurements (24).
Nutritional status was evaluated using BMI curves (Body Mass Index), weight (kg)/stature2(m), according to age, gender and the respective cut-off points proposed by Centers for Disease Control and Prevention (25) and for the American Academy of Pediatrics (26), which are: eutrophy between 5 and 85 percentiles; risk of overweight between 85 and 95 percentiles, and considered overweight or obesity =95 percentile (25,26).
The sample was subdivided into two groups using BMI criteria, one consisting of eutrophic patients, and the other consisting of at risk of overweight and obesity in patients.
Dietary evaluation consisted of a 24 hour data recording method, reporting all consumed foodstuffs including drinks over a 24h period, in all meals taken over 3 days so that consumption could be estimated. The adolescents were interviewed in the presence of one of their parents or guardians when necessary. On this occasion, they were shown how to fill in the 24h data recording chart to obtain three days records.
Foods or preparations given in other measures were converted to grams. Data on food consumed (in grams) in the diet were converted into nutrients using food chemical composition tables from Virtual Nutri, version 1.0 (1996), developed by teaching staff from the Nutrition Department, USP School of Public Health (27).
Data on foods and preparations not listed in Virtual Nutri were taken from the Endif Table of Food Composition – IBGE (28) and the home food measures table from the Nutrition Department, USP School of Public Health (29).
This study only considered calcium source foods: milk, cheeses, yogurts, cream cheese, and prepared foods. The adolescents were also questioned on their intake of substances that could interfere in its absorption, such as: caffeine drinks, soft drinks, use of exclusively vegetarian diets, and high dietary fiber. No adolescent declared a relevant ingestion of elevated fiber or vegetarian diet. Adolescents were questioned about foods that could interfere in calcium absorption as they were submitted to bone mass evaluation using bone densitometry (DEXA).
Daily calcium consumption results were presented according to gender, stage in life, and nutritional state using a threshold of 1300mg/day as recommended by the Institute of Medicine (22), where values consumed are below, equal to, or above this value. This allowed us to calculate the number of adolescents who consume less than the Adequate Intake (AI) value (22), as EAR’s and RDA’s are still not available for this nutrient (22). In addition to presenting calcium intake in mg/day represented on graphs by medians and their respective quartiles, for each gender and nutritional group, results were also obtained in relation to daily energy consumption by Ca(mg)/daily calorie consumption (30). To compare genders and eutrophic and risk of overweight/obesity groups, calcium density was presented in mg/1000Kcal to represent sample nutritional state.
Data were analyzed using Statistica version VI. Comparisons between groups were by Kruskal-Wallis analysis of variance and the Mann-Witney U test, once variables were verified as not having normal distribution by the Shapiro-Wilk test. The Spearman correlation test was used to verify the presence or lack of an association between BMI and calcium ingestion. The x2 test was used to analyze associations with gender. Statistical significance was considered at 5%.
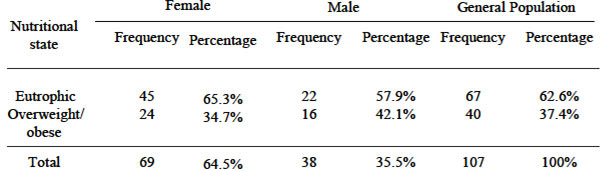
The study population consisted of 107 adolescents. 62.6% were eutrophic and 37.4% were considered at risk of overweight or obesity. Classifying by gender, 34.7% females and 42.1% males were considered at risk of overweight or obesity; data presented in Table 1.
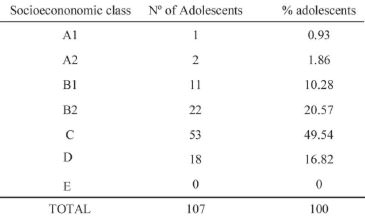
Using ANEP socioeconomic classification that varies from class A to E, Table 2, the highest number was classified in class C (49.5%) with 16.8% from class D. Therefore around 66% of these adolescents belong to low-middle income families.
In relation to the calcium consumption reference value, 86.36% of eutrophic and 87.50% classified at risk of overweight/obesity male adolescents were below the Adequate Ingestion (AI) value; we were unable to calculate lack of calcium prevalence as EAR values were not available (22). For female adolescents, 91.11% of eutrophic and 91.76% classified risk of overweight/obesity were lower than the recommended value of 1300mg/day (Table 3).
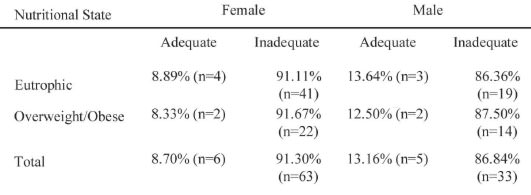
With an Al value of 1300mg/day as the split point for calcium ingestion in adolescents from both sexes and nutritional state, there was no significant difference between classifications according to gender. This indicates that nearly all eutrophic and at risk of overweight/obesity adolescents ingest less than 1300mg/day of ca1cium.
Table 4 shows ca1cium density values (mg/lOOOkcal), for the male adolescents was 356.5±159.2 mg/lOOOkcal for eutrophic and 267.8±163.2mg!1 OOOkcal for those considered overweight/obesity. Statistical analysis showed that eutrophic male adolescents had higher ca1cium densities than their at risk of overweight/obesity male peers.
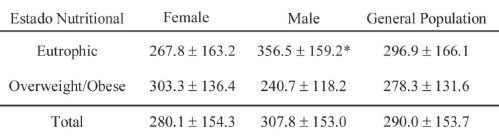
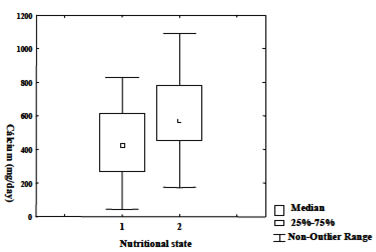
Median calcium ingestion levels were 430.9mg/day for female eutrophic and 572.7mg/day for female overweight/obesity; however for males, median ingestion was 803.1mg/day for eutrophic and 466.4mg/day for the overweight/obesity group. Graphs 1 & 2 show median and quartile distributions for eutrophic and risk of overweight/obesity groups for female and male adolescents respectively.
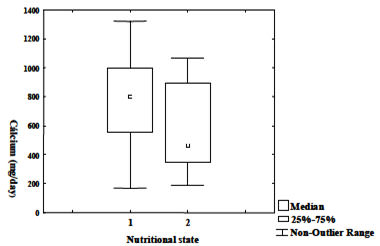
The Spearman coefficient of correlation verified a significant negative association between Calcium intake and BMI for males, r= -0.488 with p=0.0173* and nonsignificant for females, r= -0.250 with p=0.216.
Currently, obesity in children and adolescents is rising in many parts of the world; in some it is already considered to be at epidemic proportions. According to the US Surgeon General, the number of overweight children has doubled and overweight adolescents tripled in the USA compared to data from epidemiological studies from the last two decades (31).
Most of the adolescents in this study had normal nutritional status (62.6%), however it must be stressed that a high proportion (37.4%) were diagnosed as at risk of overweight/obesity. This proportion was a little higher than studies made in the USA (32) and Brazil (33), which identified values around 30%. These results agree with data from other studies made in the same department (34). Although data are taken from an outpatient clinic at a University Hospital, we stress that this clinic does not present any selection criteria, is receptive to demand, the only limiting factor is the clinic’s consulting capacity.
In a retrospective study of data obtained between 1988 and 1996 from the medical records of 469 adolescents joining the outpatient clinic between 1988 and 1992, and 258 between 1993 and 1996, the first period presented a prevalence of risk of overweight and obesity in females of 26.85% and males of 12.62%. In the second period these were 48.34% for females and 40.19% for males, indicating that levels doubled for females and trebled for males when comparing the two periods. The authors were showing that with evolution of time, these diagnoses would present elevated prevalence, highlighting an intense preoccupation as this was associated with diseases such as arterial hypertension, cardiocirculatory diseases, type 2 diabetes mellitus, osteo-articulatory diseases, neoplasias, resulting in increased mortality at increasingly younger ages (34).
In relation to estimated calcium consumption obtained from 3 days of 24h recorded data and calculating medians for both male and female adolescents (Graph 1 and 2), values were much lower than the Adequate Intake (AI) presented in DRI for this micronutrient. The adolescents had a significantly lower calcium intake than those of males, results also seen in other national and international studies (32,35).
Criticism about the form of data collection in food questionnaires is always made when this or other methods are used. However, despite significant errors reported in literature relating to this type of recording, data presented in this study were very close to those in national and international studies where results were taken from different types of food questionnaire (2,31,32,36-38).
When comparisons were made by calcium density, taking into account nutritional state and gender, significant differences were seen between male eutrophic and at risk of overweight/obesity adolescents, but not their female counterparts. According to Lee & Reicks (38), a less than recommended calcium intake can be associated with a type of breakfast, the number of children and adolescents living in the same house, possible buying power to get foodstuffs high in calcium, an understanding of this nutrient’s importance, and parents encouragement about the importance of eating foods high in calcium. Therefore when analyzing the factors which influence calcium intake in adolescents, as well as those cited earlier, there are: habits and lifestyle, limited understanding of diets, lactose intolerance, sociocultural factors and values, living with peers, media influence, etc. (8,11,13,22).
Over and above these, fat intake and concern about body shape, mainly in females, can influence lactose product intake, however Barr (39) concluded that knowledge about diet and body shape do not directly compromise calcium intake, but are associated with the type of milk selected, whether it is skimmed, semi-skimmed, or full cream (39,40).
Low calcium intake, as shown in this study, can elevate socioeconomic condition to interfere in its consumption. In a study by Silva et al (11,12) between high socioeconomic level students from Botucatu of the same age range, mean calcium intake was 863mg±280mg/day, better than in this study, but still a long way off AI values. Santos et al (41), in a study with students in Ouro Preto, demonstrated that calcium intake in a school from the highest socioeconomic level (782.02mg/day) was much higher than in a state school with a much lower level (563.20mg/day). Although different studies highlight the variability of mean daily calcium intake in adolescents, most of them reveal that consumption is less than adequate, demonstrating a worrying problem in relation to adolescents and their future bone health situation, as the bone mass accumulation rate contributes to around 50% of bone mineral content, incorporating approximately 1000g of bone mineralization during adolescence (11,12,35).
According to a study by Albano (37) at the Applied Teaching School, Education Faculty, USP, mean calcium consumption for males was 819.68mg/day reaching 63.05% of the DRI recommendations (22) for females it was 579.86mg/day, reaching 44.6% of that recommended; these are just higher than values in our study, but still inadequate.
In light of these observations, insufficient calcium intake is the result of low consumption of calcium rich foods, such as milk and its derivates, ignored by the frequent and high intake soft drinks and a proven association with low calcium intake (2,42). Although soft drink consumption was not the specific objective of this study, studies have shown that lactose drink consumption is inversely proportional to soft drink consumption (42). Whiting et al (43) found that the association between soft drinks and low calcium intake by adolescents was negatively related to bone mineral density in adolescent girls between 10 and 14 years old.
Changes in eating habits seen in American adolescents over a 30 year period have reported that they have increased their soft drink consumption, with a discrete reduction in calorie intake from proteins and fats, and have detected a drop in calcium intake where only 20% of girls and about 30% of adolescents reach the recommended levels, due to the drop in consuming milk and its derivatives (2), which have been replaced with soft drinks and juices.
Adolescents who consume large quantities of soft drinks ingest less than 20% of the calcium of those who do not. And soft drinks containing caffeine increase calcium excretion in urine, and are therefore harmful to an adequate calcium balance (11,38).
Ninety one percent of the male adolescents and 86.84% of the female members in this study presented low calcium intake, which was always below that recommended by AI. Comparing girls with different nutritional states, those who were overweight or obese presented low calcium intake when calculated in mg/1000Kcal; the same was found by Andrade et al (44), Phillips, and many other authors (30). These differences relative to males and nutritional state were also seen data were presented as medians and quartiles, as seen in Graph 2.
Scientific literature has recently suggested that low calcium intake could act as a contributory factor in the rise in obesity, and be associated to the risk of hypertension and insulin resistance syndrome (IRS) (42). This was suggested by CARDIA (7) who showed that adequate consumption of milk and its derivatives was inversely proportional to appearance of all the signs and symptoms of IRS, including obesity. Animal studies have proved, which also seems plausible in humans, that when energy intake and physical activity are under control, body fat will be less in those consuming more calcium. Heaney (10) evaluated 348 young women and saw that when their calcium intake was below the 25th percentile, obesity prevalence was 15%, however when their calcium intake was at DRI recommended levels, this prevalence dropped to 4%.
In 2004, Zemel et al. (9) prescribed 32 obese adults with three different diets, one with restricted calories, another with restriction but with calcium supplement, and the third with restriction but with lactose product supplement. All groups lost weight in different proportions; 6.4% for the calcium supplemented group, 8.6% for the restriction only group, and 10.9% for the lactose product supplement group. Physiological explanations showed that parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D regulate intracellular calcium, so diets with low calcium intake stimulate PTH and 1,25-dihydroxyvitamin D, which in turn favor intracellular calcium uptake in adipocytes, stimulating lipogenesis and inhibiting lipolysis (9). Another mechanism cited as having a possible effect from calcium intake on not gaining weight or body fat, seems to be its bonding to fatty acids in the colon which inhibit fat absorption and activate fat excretion (45).
As many authors have highlighted adequate calcium intake as a protection factor in preventing the occurrence of obesity and others have contested this fact (9,10,19,40,42-47), there is a pressing need for its role to be clarified especially as adolescence is the time of life when a large amount of bone mass is acquired, its importance in boosting bone mineral build up is unquestionable, but other studies are needed to clarify its possible relationship with excessive weight gain when consumed in lower than recommended doses. It must be said that, even though some of its action mechanisms have been clarified, authors reinforce the importance of adequate intake, above that recommended, for effective calorie restriction in helping prevent obesity. So there is still some speculation of how to transfer some of these hypotheses when working with humans, in conditions of food consumption freedom (9,43).
This study showed that a low consumption of calcium rich foods by adolescents translates into a lower than recommended intake of this micronutrient in this population when values are compared with recommended DRI for calcium (22).
Evidence from this study that insufficient calcium intake correlated to the risk of excessive weight gain in male adolescents, emphasizes that eating foods with adequate nutritional value, supplemented by helpings of calcium rich food which favor the prevention of obesity and its comorbidities, also help gain adequate bone mass which is responsible for bone health in later years.
Even with these facts stating that low calcium intake increases the prevalence of obesity in female adolescents, was not proved in this study, it seems desirable that guidance on adequate calcium intake is emphasized for both sexes due to the serious health problems resulting from inadequate intake.
Ilana Lederer Goldberg Coutchie and Stuart Coutchie for the English translation of the Abstract.
Recibido: 10-06-2008
Aceptado: 22-09-2008