The objective was to assess the relative validity of a food frequency questionnaire (FFQ) to estimate daily vitamin A intake in pregnant women using two biomarkers as references, maternal serum retinol and breast milk retinol. This is an observational, descriptive, analytical, cross-sectional study. FFQ was applied to 161 pregnant women at the largest public maternity hospital in Ribeirão Preto, Brazil. The FFQ recall period was the last 30 days before childbirth. The mother was asked if she had consumed or not each food item over the last 30 days, how often and which portion size. Samples of maternal blood and breast milk for determination of retinol concentrations were collected. Partial Pearson correlation test, agreement by kappa quadratic statistics, cross-classification into quartiles and the method of triads with two biomarkers were performed. The mean FFQ intake of vitamin A was 875 µg/day and the frequency of inadequate intake was 52.8%. Low correlation coefficients were observed between the FFQ and both biomarkers. In cross-classification, considering foods sources with or without provitamin A, 63.6% to 68.3% of the results fell into the same or adjacent quartiles, respectively; less than 10% of all results were classified into opposite quartiles. The validity coefficient of the FFQ was 0.484. FFQ performed better when considering only food sources of preformed vitamin A and both biomarkers (ρ=0.554). As a conclusion, FFQ provided an estimate of vitamin A intake with moderate accuracy, being suitable to rank pregnant women according to categories of intake.
Key words: Food Consumption, validation studies, vitamin A, pregnant women, nutritional status
O objetivo foi avaliar a validade relativa de um Questionário de Frequência Alimentar (QFA) para estimar o consumo de vitamina A em mulheres grávidas usando dois biomarcadores como referência, retinol sérico materno e retinol de leite materno. Trata-se de um estudo observacional, descritivo, analítico e transversal. O QFA foi aplicado a 161 gestantes na maior maternidade pública de Ribeirão Preto. O período de abrangência do QFA foi de 30 dias antes do parto. Questionava-se à mãe se ela havia ingerido ou não cada item de alimento contido em um álbum fotográfico nos últimos 30 dias e qual era a frequência e o tamanho da porção consumida. Foram coletadas amostras de sangue materno e leite materno para determinação das concentrações de retinol. Foi realizado o teste de correlação parcial de Pearson, concordância de kappa, classificação cruzada em quartis e o método de tríades com dois biomarcadores. A ingestão média pelo QFA de vitamina A foi de 875mg / dia e a frequência de ingestão inadequada foi de 52,8%. Baixos coeficientes de correlação foram observados entre o QFA e ambos os biomarcadores. Na classificação cruzada, considerando fontes de alimentos com ou sem provitamina A, 63,6% a 68,3% dos resultados caíram no mesmo quartil ou adjacentes, respectivamente; Menos de 10% de todos os resultados foram classificados em quartis opostos. O coeficiente de validade do QFA foi de 0,484. O QFA apresentou melhor desempenho quando considerou apenas fontes alimentares de vitamina A pré-formada e ambos os biomarcadores (ρ = 0,554). A acurácia do QFA para a estimativa de vitamina A foi considerada moderada, sendo adequado para categorizar as gestantes em categorias de consumo.
Palavras chave: Consumo de alimentos, estudos de validação, vitamina A, gestantes, estado nutricional.
1 Ribeirão Preto Medical School, University of São Paulo, Ribeirão Preto, Brazil. 2 Federal University of São Carlos - UFSCAR, São Carlos, SP, Brazil.
The human embryo depends exclusively on the maternal circulation retinol for its vitamin A supply; it reaches the embryo through the maternal-fetal barrier, that is, the placenta and the yolk sac. In general, circulating retinoid concentrations reflect maternal vitamin A status, which is determined by both the inventories and recent intake; therefore, changes in these concentrations affect the amount of vitamin A available to cross the placenta and reach the fetus (1). This transfer is fundamental since vitamin A has an important role in the processes of cell differentiation and growth of the fetus and is necessary for the development of several organs such as lungs, heart, kidneys and eyes (1). In addition, retinol also plays an important role in early embryo development, skeletal and spinal cord formation, and other neural structures. The extreme deficiency of this micronutrient during pregnancy can lead to the so-called vitamin A deficiency syndrome, characterized by cardiac, pulmonary, skeletal and urinary tract ocular malformations (2). Maternal vitamin A status before and during pregnancy influences its levels in breast milk and in the newborns (3); breast milk is the only source of vitamin A for exclusively breastfed infants (4). Poor vitamin A intake is the primary cause of vitamin A deficiency (VAD), a leading nutritional problem worldwide, which is associated with increased maternal and infant morbidity and mortality (5).
The assessment of dietary intake by appropriate methods is a great challenge in research on health and nutrition. The food frequency questionnaire (FFQ) is a widely used tool for the assessment of food intake at the population level. However, FFQs developed for different population groups have been used to estimate the intake of pregnant women (6) since FFQs developed and validated for this population are still scarce in the scientific literature (7).
The validity of an FFQ is defined by the degree of accuracy with which this method measures the dietary aspect for which it was designed. The lack of a gold standard to estimate food consumption motivates the search for better methods of evaluation.
The method of triads (7) has been used to determine the accuracy of the FFQ compared to the estimate obtained by 24-hrecalls or food records and biomarkers. Due to the high intraindividual variability of vitamin A, 19 replications of 24-h recall or food records would be required to estimate the intake during the pregnancy, which would make the use of these methods unfeasible for population studies (8).
In this context, biomarkers have been presented as a potential gold standard in validation studies, since errors generated by them are not only related to ingestion, but also to metabolism. It is important that the compared methods present errors as independent as possible (8). Applying two biomarkers in the same triad seems to be useful regarding measurement errors, but it’s still uncommon (9).
The aim of this study was to assess the relative validity of a FFQ for estimating vitamin A intake using biomarkers as references in pregnant women.
This is an observational, descriptive, analytical, cross-sectional study. Pregnant women seen at the largest maternity hospital (Centro de Referência de Saúde da Mulher – Mater) of Ribeirão Preto (SP, Brazil) participated in this study. Data were collected between August and October 2012. One hundred sixty-one mothernewborn pairs were selected since the mother had completed FFQ data. Additionally, mothers’ blood and breast milk were obtained in order to determine retinol concentrations. This sample size is considered suitable for validation studies including biomarkers (10).
Inclusion criteria were healthy women aged between 18 and 39 years old (median: 24 years old), mothers of a single healthy fetus born by vaginal or cesarean delivery at term (gestational age between 37 and 42 weeks), with birth weight greater than 2500 g. Exclusion criteria were women under 18 years old, seropositive mothers for human immunodeficiency virus (HIV), mothers with diabetes mellitus, hypertension, lung disease, heart disease, acute infection or bleeding with hemodynamic instability, and premature newborns or term ones with low birth weight, twins, with asphyxia, meconium aspiration or congenital abnormality.
The present study was approved by the Ethics Committee in Research of the University Hospital, Medical School of Ribeirão Preto, Brazil (number 388.724/2013).
Maternal blood was collected during the initial admission in the antepartum room. Some obstetric and anthropometric data of the mother and newborn were obtained from the medical records or during the postpartum interview, when the mother had already returned to her room.
Breast milk samples (about 1 to 2 ml of colostrum) were collected the day after delivery and before discharge, by manual milking of either breast (if necessary, milking was done on both breasts, until the minimum volume (1 ml) of milk was obtained). On that occasion, the mother also responded to the FFQ.
Both blood samples and colostrum samples were collected in tubes protected from light to prevent photodegradation of vitamin A. After collection, blood samples were centrifuged in the maternity laboratory and the serum was separated and frozen at -70 °C, until the moment of the analyzes. Colostrum samples were immediately frozen after collection at -70 °C until the time of analysis.
Samples of blood and breast milk were analyzed at the Laboratory of Nutrition and Metabolism, Department of Internal Medicine, Medical School of Ribeirão Preto, University of São Paulo. Both samples were analyzed by HPLC. The procedure proposed by Arnaud et al. (11) was used for the serum samples and a technique from Giuliano et al. (12) adapted by Ribeiro et al (13) was used for the breast milk samples. The cutoffs for VAD were 0.70 µmol/L for maternal serum retinol and 1.05 µmol/L for breast milk retinol (5). The Institute of Medicine criteria was employed to assess pre-pregnancy BMI adequacy (14) and adequacy of BMI was evaluated according to gestational age (15).
Vitamin A intake was assessed by the Simplified Dietary Assessment (SDA) developed by the International Vitamin A Consultative Group (IVACG), previously adapted to the Brazilian population (16) but not previously validated.
The present study applied a FFQ with 32 items based on the list of potential food sources of vitamin A and carotenoids described by Tuma (16). Some foods were grouped into the same item, e.g. raw kale and stewed kale.
The FFQ recall period was the last 30 days before childbirth. The mother was asked if she had consumed or not each food item over the last 30 days, how often and which portion size. An album with colored pictures of small, medium and large portions of food sources of vitamin A (arranged from top to bottom, a page for each food item), developed by Tuma (16) was used to illustrate the portion sizes, characterizing the questionnaire as semi-quantitative. The mother was asked to point at the picture that was closest to the portion size she had consumed.
Calculation of vitamin A intake using the FFQ
The measurement of vitamin A from data collected with the FFQ was based on the Food Composition Database of the Brazilian Household Budget Survey 2008-2009 (17). For foods which the unit was retinol equivalents (RE), conversion was performed to retinol activity equivalents (RAE) by dividing the value by 2. The medium and larger portion sizes were considered two and three times larger than the small size, respectively (16). Calculations were performed using Microsoft Excel 2010 software and results are reported as RAE/day. The use of supplements during pregnancy was also considered and the amount was added to the intake when a supplement containing vitamin A was reported. Intake values <550 µg RAE were considered inadequate (18).
Descriptive characteristics were presented as mean and standard deviation, and as absolute frequency and percentage. The average income was calculated according to the number of minimum wages in the state of São Paulo in 2012. The Brazil Criteria of economic classification (19) was used.
The Pearson correlation test was applied to determine the correlation between biomarkers and between each biomarker, i.e., maternal serum retinol or breast milk retinol, and estimated vitamin A intake from the FFQ. The amount of vitamin A from supplements was added to the vitamin A intake in a second application of the test in order to determine if the supplement would be an adjustment variable. Additionally, the FFQ was tested to estimate preformed vitamin A, including only foods of animal origin (cakes were excluded). Additional variables were tested as adjustment for the partial correlation analysis. Quadratic kappa statistical analysis and rossclassification into quartiles were performed to assess the agreement between the FFQ and the biomarkers. All data were log transformed prior to analysis.
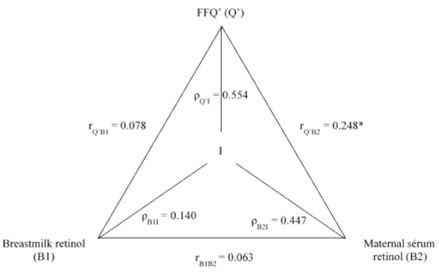
The method of triads (20) was used to estimate the validity coefficient between the real intake (unknown) and the estimated intake obtained by the FFQ and two biomarkers. Originally, that method is a triangular comparison of an FFQ, a biomarker and reference methods, the latter being 24-hour recall or food record. The validity coefficient is calculated according to the following equations:
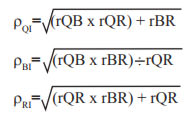
where ρQI, ρBI and ρRI are validity coefficients between the real intake (I) and the FFQ (Q), the biomarker (B), and the reference method (R), respectively; and rQB, rQR and rBR represent the correlation between the biomarker and the FFQ, the FFQ and the reference method, the biomarker and the reference method, respectively. In the present study, two biomarkers were used instead of only one with the reference method.
One hundred sixty-one mother-newborn pairs completed the FFQ and were therefore included in the study. Maternal serum retinol was obtained from all 161 mothers and 140 milk samples were obtained for the determination of retinol; in 21 cases collection was not possible (grounds for refusal or lack of material for laboratory analysis).
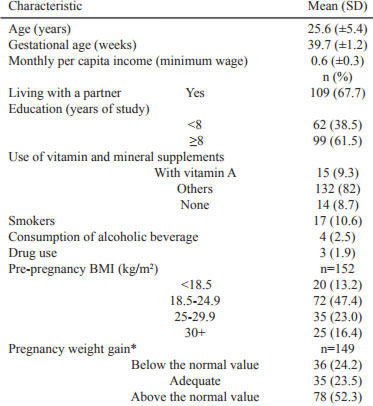
Table 1 describes the maternal sociodemographic characteristics, nutritional status and lifestyle. On average, gestational age was 39.7 weeks and mothers were 25.6 years old, reported living with a partner, earned a little more than half the current minimum wage, had at least full elementary education and did not report a risky lifestyle (smoking, alcohol drinking and drug use); most of the mothers had consumed one type of vitamin or mineral supplement but without vitamin A. Additionally, most of the mothers were of normal weight prior to pregnancy, 52.3% showed a larger weight gain relative to their pre-pregnancy weight, and mean gestational weight gain was 14.3 kg.
The median estimate of dietary vitamin A alone was 500.3 μg RAE/day. When considering the vitamin A content of the supplements, the median estimate was 571.8 μg RAE; in both cases the estimate ranged from 51 to 7205 μg RAE. The FFQ was also applied considering only the items containing vitamin A of animal origin (preformed vitamin A), which included only 9 food items: fried beef liver, mozzarella cheese, fried fish or fish cooked with a sauce, fried egg or omelet, whole milk, fried chicken, butter, margarine and cheese curd. In both cases, vitamin A values ranged from 17 to 7195 μg RAE and the median was 265.8 μg RAE.
Eight (5.0%) mothers had an estimated level of vitamin intake above the tolerable upper intake level (UL), ie, 3000 μg RAE(21), but none of these cases was due to the use of supplements. These data were not excluded. Eight-five mothers (52.8%) had a vitamin intake below that recommended (550 μg RAE) (21). The proportion of mothers with a vitamin intake (only dietary) below the EAR and simultaneously serum retinol ≤0.70 μmol/L was 32.9%.
The mean concentrations of maternal serum retinol and breast milk retinol were 0.66 μmol/L (SD:±0.26 μmol/L) and 2.97 μmol/L (SD:±0.27 μmol/L), respectively. Thirty-six percent of the maternal blood samples had a serum retinol content considered marginal (>0.70 μmol/L and <1.05 μmol/L), and 55.3% of the mothers had VAD (serum retinol ≤0.70 μmol/L). Regarding the milk samples, 27.1% had retinol concentrations <1.05 μmol/L. After logarithmic transformation of the variables with non-normal distribution, the Pearson correlation coefficient was calculated between breast milk retinol and maternal serum retinol (r=0.063).
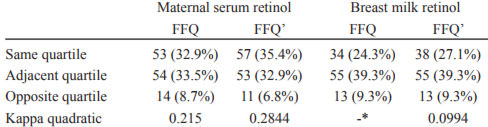
Cross-classification analysis between the FFQ and each biomarker revealed both a decrease in the proportion of rating on opposite quartiles and a slightly higher kappa agreement when only preformed vitamin A was considered (Table 2).
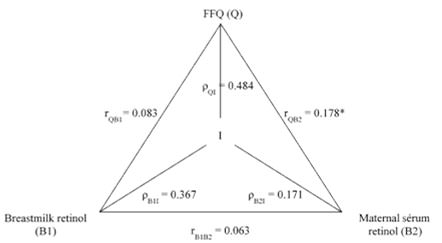
Figures 1 and 2 present the results of FFQ analysis by the method of triads - with all items (carotenoids and retinol food sources) and with only preformed vitamin A food sources, respectively. The best validity coefficient for the FFQ was obtained in the triangular comparison between the biomarkers of retinol in breast milk and in the mother’ serum when only preformed vitamin A food sources were considered.
The The objective of the present study was to validate the use of an FFQ to estimate the intake of vitamin A in pregnant women seen at the largest public maternity of Ribeirão Preto, Brazil.
Despite the high frequency of inadequate intake, the FFQ estimated an average intake of vitamin A of 875 μg/day, higher than the value recommended for pregnant women (EAR: 550 μg RAE; RDA: 770 μg RAE). It should be pointed out that 8 mothers (5.0%) had an estimated vitamin intake above UL (3000 μg RAE) and their data were not excluded from the analysis. These levels were associated with consumption of beef liver, which contains a large amount of preformed vitamin A.
In the present study, although 50% of the mothers reported excessive weight gain during pregnancy, 52.8% had an inadequate intake of vitamin A; moreover, 55.3% of mothers had serum retinol ≤0.70 μmol/L and 27.1% presented retinol concentrations <1.05 μmol/L in breast milk. The IBGE Institute of Statistics family budget surveys (17) carried out the first Brazilian National Dietary Survey and observed a high prevalence of inadequate intake of micronutrients in the overall population, including a high prevalence of inadequate nutrient intake in pregnant women and also in women of reproductive age: for vitamin A, 71% vs. 72%, respectively. Brazilian women do not change their food consumption during pregnancy in order to reach the increased nutritional goal (22). As reported by the IBGE, Brazilian women have a high consumption of foods with a high-energy content and a low micronutrient content (17).
It was observed that the FFQ presented a moderate accuracy for the estimate of vitamin A intake by the mothers under study. An additional analysis was performed considering only the food sources of preformed vitamin – which has better bioavailability than provitamin A -, revealing a better performance of the questionnaire. In this analysis, maternal serum retinol was the biomarker that best estimated vitamin A intake (Figures 1 and 2).
In general, the inclusion of vitamin A content from supplements did not improve the correlation coefficients. The same occurred when only preformed vitamin A was considered. Low correlations (less than 0.4) were expected since various factors influence the concentrations of these markers far beyond the nutrient intake, such as absorption, metabolism and physiological regulation (20). However, the correlations between the FFQ estimated vitamin A and biomarkers in the present study was higher than the verified in previous studies conducted among pregnant women in Brazil(23) and Japan(23). In a review of validation studies of FFQs, which included 164 papers, Cade et al. (2004) described that the mean correlation between the estimative of vitamin A (from FFQ) and weighted records was 0.39; when unweighted records and food recalls were used as the reference methods the mean were 0.38, and 0.39, respectively. Finally, when biomarkers were used as the reference method, the mean correlation was 0.35. Regarding the transfer of retinol to human milk, there are still many unknown stages of the process and, therefore, a linear relationship between the vitamin A concentrations in blood and maternal milk cannot be accepted. These observations may help explain the results observed in the present study.
The scientific literature recommends that agreement tests be applied in addition to the correlation tests and considers as desirable results that indicate over than 50% of subjects being correctly classified, less than 10% misclassified into opposite quartiles and kappa values above 0.4 (24). The present results (Table 2), when considered in the same quartile or adjacent quartile, indicate that the proportion exceeds 60% for any comparison. Low agreement kappa values and a satisfactory result in cross-classification may be related to the distribution of data into quartiles: data close to the cutoff point may be in different quartiles; likewise, data far from each other may be classified in the same quartile (24). This characteristic may influence the correlation values, especially if the sample size is small; this is a limitation of the present study
The use of biomarkers for reference purposes in the method of triads has an advantage since there is no relationship between the errors measured by them and the measurement errors that occur in dietary investigations. However, the literature indicates that this advantage applies only to recovery biomarkers. Biomarkers of concentration, such as vitamin A (retinol and carotenoids) generally do not have the same quantitative relationship with food intake for all individuals; therefore, their results cannot be transformed into an absolute intake per unit of time. This kind of biomarkers only provides a correlation with food intake. However, the method of triads has been applied in the literature even when using biomarkers of concentration (25). Adjustment for energy could be an alternative to reduce random error when the FFQ provides this type of information (26), although this was not available in the present study. It should be noted that, in the absence of a gold standard for the assessment of dietary intake, validating the FFQ is considered relative(8, 10).
The use of two biomarkers in the same triangular comparison rather than just one excludes the use of a recall or food record, which is used to reduce the intra- and interpersonal variations. Vitamin A is a nutrient with high individual variability and therefore multiple dietary recalls would be needed to obtain the habitual intake of this micronutrient, with a more difficult process of data collection. Moreover, despite the increased cost of analysis, using two biomarkers may be more advantageous regarding measurement errors (9). Biomarkers have been used separately in distinct triangular comparison analysis; however, the use of two biomarkers in the same triad is exceptional in the scientific literature and has been shown to be an important complement in assessing food intake (27).
A study conducted with 119 Norwegian pregnant women (27) collected urine and blood samples for analysis of flavonoids and carotenoids, respectively. The highest validity coefficient of the FFQ was 0.65 for citrus fruits or juice in a triangular comparison with hesperetin and zeaxanthin and the lowest was 0.37 when the FFQ was compared with phloretin and alphacarotene. In the cross-classification, about 60% of the participants were correctly classified when the FFQ and biomarkers were compared (27). Another study compared two biomarkers (plasma carotenoids and urinary flavonoids) in the same triad but not conducted with preganant women and detected a validity coefficient for the FFQ ranging from 0.6 to 0.94 (25). This fact may be related to the items of each FFQ and to the application of the questionnaire during the interview, which, in the present study, was conducted during the immediate postpartum period, when mothers may have had some kind of recall bias.
An important limitation of using the method of triads in this study is that both biomarkers might be subject to the same type of error because the same micronutrient was measured in different biological samples. Moreover, both biomarkers were determined by HPLC. Furthermore, although the process of retinol transfer from blood to human milk is not fully known, there must be a relationship between the micronutrient concentrations in the two fluids.
Lack of 24h-recall or food records is another limitation of the present study; however, as it was mentioned earlier, 19 replications of 24-h recall would be required to estimate the intake during the pregnancy, which would make the use of these methods unfeasible for population studies.
Regarding vitamin A, some considerations must be made about its metabolism. Serum retinol dosage has a good correlation with the body’s reserves when the results are lower than 0.70 μmol / L or higher than 1.05 μmol / L, but it has a limited value in diagnosing VAD in intermediate values (28). In addition, if not used immediately, dietary retinol may be stored in the liver in star cells (29); thus, serum retinol concentrations may not reflect recent intake of the micronutrient. It is also known that colostrum naturally contains higher concentrations of retinol than the transition and mature milks (30). These observations need to be taken into account in the interpretation of the data when a micronutrient with these characteristics is used and may constitute a limitation of the study.
Finally, it is necessary to point out that pregnancy is a unique period in which important changes occur in the female organism. Pregnant women have plasma volume expansion of 45% on average, which changes the concentrations of serum proteins and hormones (31). This fact has to be considered. Thus, not only the nutritional status of pregnant women but also the gestational period during which their vitamin A status is assessed should be taken into account.
More studies in the nutritional area are needed, especially about the methodology of food intake assessment. New methods and new types of statistical analyses considering factors inherent to pregnancy – such as plasma volume expansion - should be developed in order to obtain more accurate results consistent with reality. Assessment of food intake will always be a challenge.
The FFQ permitted a moderately accurate estimate of vitamin A intake in pregnant women, especially when only preformed vitamin A food sources were considered. Since a high proportion of women classified correctly into the same or adjacent quartiles, we conclude that the FFQ was suitable to rank pregnant women according to categories of intake.
The authors would like to thank the Maternity Hospital “Centro de Referência em Saúde da Mulher – Mater”, Ribeirão Preto and the Laboratory of Nutrition and Metabolism, Ribeirão Preto Medical School, University of São Paulo. We would also like to thank “Coordination for the Improvement of Higher Education Personnel” (CAPES, Brazil) for the financial support (scholarship sponsor) of this study.
Recibido: 20-08-2017
Aceptado: 05-10-2017