Childhood obesity is a major public health issue in Mexico. Schools are important settings to promote healthy eating habits. The aim of this study was to assess the extent of compliance with 2010 and 2014 Mexican school food guidelines in six public primary schools in Mexico City. The instruments for this study included semi-structured interviews (n=17) with principals, food vendors and members of the School Vending Committee, focus groups (n=10) with teachers and with parents, observation of six schools’ environments, questionnaires applied to 325 schoolchildren from 4th, 5th and 6th grades and their parents, and a food analysis of items sold at school vending. Guidelines’ compliance was assessed using all instruments accordingly. It was low in every dimension: 1) Acknowledgment of school food guidelines: None of the participants were familiar with the 2014 guidelines. 2) Healthy environment enhancement: Children lacked free access to safe drinking water. Children had up to five opportunities to eat during school day besides breakfast at home. Most children (67.7%) ate three to four times. 3) Operability of food and beverages sale and consumption: The only training provided to stakeholders was an annual session on hygiene to school food vendors. The majority of food and beverages offered at school vending exceeded energy, sodium, fat and added sugar content as established. Children sold energy-dense foods for school fundraising. Lack of dissemination and acknowledgment of the guidelines, defined roles and policy procedures, as well as training and capacity building for stakeholders impeded school food guidelines’proper implementation. Arch Latinoam Nutr 2019; 69(4): 209-220.
Key words: Food guidelines, food policy, school vending, scholars, primary schools
La obesidad infantil es un problema de salud pública en México. La escuela es un lugar importante para promover hábitos saludables. El propósito del estudio fue evaluar el cumplimiento de los lineamientos escolares de alimentos de 2010 y 2014 en seis escuelas primarias públicas de la Ciudad de México. Los instrumentos incluyen entrevistas semi-estructuradas (n=17) con directores, vendedores de alimentos y miembros del Comité del Establecimiento de Consumo Escolar, grupos focales (n=10) con padres y con profesores, observación del entorno escolar, cuestionarios aplicados a 325 niños de 4º, 5º y 6º grado y a sus padres, y un análisis de los alimentos ofrecidos en la venta escolar. El cumplimiento de los lineamientos fue bajo en cada dimensión: 1) Conocimiento de los lineamientos: Ninguno de los participantes conocía los lineamientos de 2014. 2) Promoción de un ambiente saludable: No se tenía acceso libre a agua simple potable. Los niños tenían cinco oportunidades para comer durante la jornada escolar además del desayuno en casa. La mayoría de los niños (67.7%) comía de 3 a 4 veces. 3) Operatividad de la venta y consumo de alimentos y bebidas: La única capacitación fue una sesión anual de higiene a los vendedores. La mayoría de los alimentos y bebidas excedía los límites establecidos de calorías, sodio, grasa y azúcar añadida. Los niños vendían alimentos densos en energía para recaudar fondos. La falta de difusión de las guías, roles y políticas no definidos y una mínima capacitación obstaculizaron la implementación de los lineamientos. Arch Latinoam Nutr 2019; 69(4): 209-220.
Palabras clave: Lineamientos de alimentación, políticas de alimentación, cooperativa escolar, escolares, escuelas primarias
https://doi.org/10.37527/2019.69.4.002
Autor para la correspondencia: Mario E. Rojas-Russell, email: [email protected]
Childhood obesity is one of the main public health issues in Mexico. According to the last National Health and Nutrition Survey (Encuesta Nacional de Salud y Nutrición 2018) over a third of Mexican schoolchildren (35.6%) are overweight or obese (1). Childhood obesity is difficult to treat, while the risk of being obese and to develop chronic diseases increases during adulthood (2).
School is considered an important setting to promote healthy eating habits in children (3). Most Mexican children enrolled in the public school system go to school for four and a half hours,which accounts for a third of the time they are awake. During this period, two mealtimes are scheduled: a government-subsidized breakfast for vulnerable populations and recess in the middle of the school day. In the latter, children are allowed to bring food from home and/or buy food and beverages from school vending. Research has found that food preparations and snacks contribute the most to children’s energy intake from school vending (4). A previous study found that Mexican children may have up to 5 opportunities to eat by the end of the school day (5).
In 2010, school food and physical activity policies were issued for the first time in Mexico, aimed to promote a healthy school environment. The Agreement by which general guidelines for food and beverage sale and distribution are established at basic education food facilities was part of the National Agreement for Healthy Eating: Strategy against overweight and obesity (6). It included nutrition standards for food sale during recess and responsibilities for each school stakeholder to enhance compliance. It was planned to be gradually fulfilled in three stages. The first stage (SI) was scheduled to be applied from January to July 2011; second stage from August 2011 to July 2012 (SII); and third stage from August 2012 onwards (SIII).
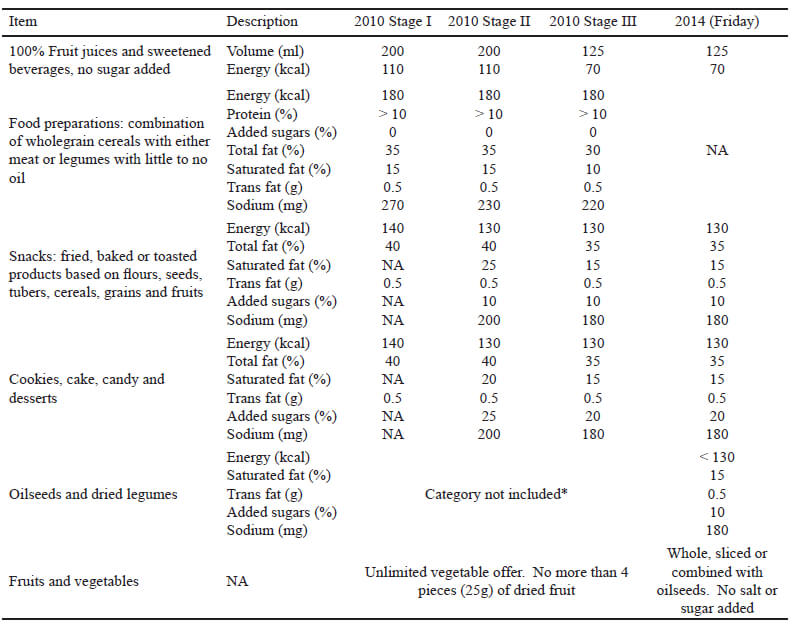
In 2014, an update to the school food guidelines was issued (7). Only fruits, vegetables, legumes and oilseeds were allowed to be sold from Monday to Thursday at recess, while on Friday it was also allowed to sell snacks and cookies, cake, candy and desserts. Standards for the categories available on Fridays were very similar to those from the 2010 guidelines’ SIII. However, the 2014 guidelines standards separated nuts, seeds and legumes as a new category (previously considered as snacks) and food preparations were no longer included. Another relevant change for the 2014 guidelines was the school stakeholders’ roles. Training, nutritional counseling to parents and conformation of the School Vending Committee (SVC) were the most relevant modifications.
This is the first study to assess compliance of foods offered at school vending, including a qualitative design to explore the school stakeholders’ experience regarding 2010 and 2014 guidelines’ implementation. Prior studies had evaluated guidelines’ availability at schools, compliance of snacks brought from home versus bought at school and compliance with nutrition standards (4,8,9,10).
Qualitative and quantitative instruments were used to provide a comprehensive assessment of school food guidelines’ implementation. A pilot study was conducted from March to May 2014 at one primary school to test initial design and instruments. As 2014 guidelines were released on May 2014, becoming the normativity in force since August 2014, it was decided that both 2010 and 2014 guidelines would be considered. Data were collected in six public primary schools from one municipality (representing 26% of schools from that municipality) in Mexico City, from September 2014 to May 2015. Written consent was obtained from parents and verbal consent from the other stakeholders. Ethic standards were followed according to the Declaration of Helsinki and the National Autonomous University of Mexico (UNAM) Ethics Committee.
Six schools were chosen randomly from a sample of 84 schools. Principals, teachers, food vendors and members of the SVC from each school were purposefully selected. Students enrolled in 4th, 5th and 6th grade and their parents were invited through written messages sent home and posters hung outside the schools. These school grades were chosen based on the children’s ability to answer the questionnaires.
Observation of the school food environment was registered on field notes. Food sale was observed at each school for one week. Semi-structured interviews were conducted with the principal, one food vendor (out of an average of 9 vendors) and one member of the SVC from each school. Data from onet eachers’ focus group was taken as an SVC interview for a school, as several SVC members discussed it in depth. Ten focus groups were conducted; five with parents (an average of 6 per focus group), and five with teachers (an average of 7 per focus group). Data from the focus groups showed similar patterns in the first five schools, and no new information was expected to be retrieved. As data saturation was reached, focus groups were not conducted on the sixth school.
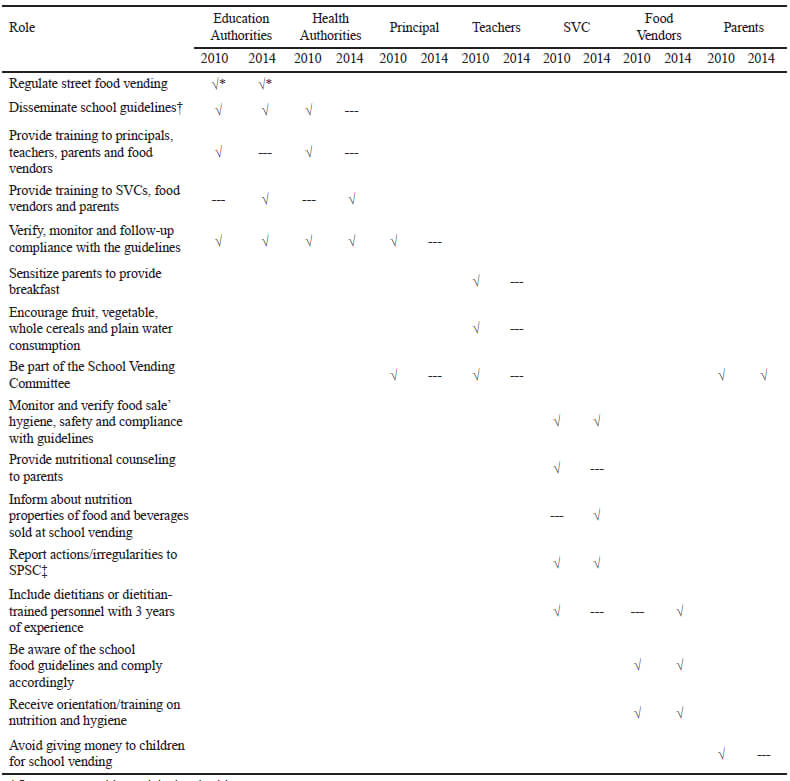
Guides for focus groups and semi-structured interviews were based on the 2010 and 2014 school food guidelines, including school stakeholders’ roles available in Table 1 (6,7). Focus groups and semi-structured interviews were audio-recorded and transcribed.
Questionnaires were administered to children to explore their dietary habits at school. Additionally, one parent of each child answered a questionnaire to determine socio-demographic characteristics.
A sample of each food item available for sale at recess was collected at each school on a Friday, as both 2010 and 2014 guidelines would apply. Each item was identified, described and weighed.
A qualitative content analysis approach was used (11). Three dimensions were derived from the data: 1) Acknowledgment of school food guidelines, 2) Healthy environment enhancement and 3) Operability of food and beverages sale and consumption. These are available in Table 2.
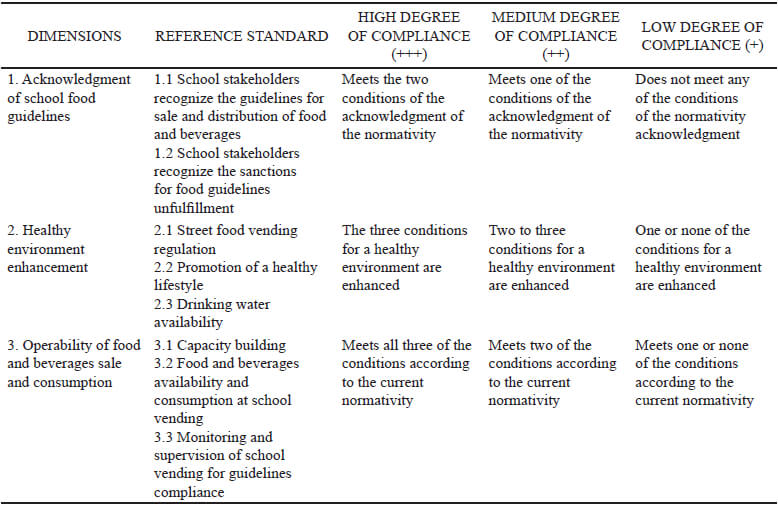
The process was as follows: a list of codes was developed from those theoretically identified for 2010 and 2014 guidelines’ compliance, adding those that emerged from the data. After the integration of a thematic matrix, categories and subcategories were determined. A triangulation of observation, survey data and testimonies of key school informants was performed after information systematization. Implementation assessment was performed using the Fidelity outcome proposed by Proctor (12). Reference standards were integrated according to the elements of the implementation to be evaluated, and a degree of compliance was developed for each dimension.
Socioeconomic status (SES) was calculated using the AMAI 8X7 scale (13). Frequency distributions were obtained from the children’s questionnaire.
Each food item was classified according to the corresponding food category. Criteria for each food category is shown in Table 3. Food sale analysis was conducted to determine energy and nutritional content by using the USDA Food Composition Database (14), the Mexican Equivalent Food System (15) and nutrition labels of pre-packaged food.Compliance with 2010 guidelines’ SI and SIII, as well as 2014 guidelines’ standards (Table 3) was determined by venue, for each item, using a binary response (0=does not comply, 1= complies) on complete fulfillment of criteria. SII was not considered since its food standards did not differ significantly from SI and SIII.
Six school food environments were assessed. Questionnaires were administered to 325 children and their parents. Participants ranged from 44 to 62 children per school, which represented 8.5% to 21.2% of the student population. There were more females (53%) than males (47%). The majority of the families (70%) fell under a low SES, while a quarter (25%) belonged to a medium SES and only 5% had a high SES.
There was a low degree of compliance on the three assessed dimensions at all schools: Acknowledgment of school food guidelines, Healthy environment enhancement and Operability of food and beverages sale and consumption.
Principals, teachers, SVC members, food providers and parents were not aware of the 2014 guidelines.One teacher declared that “unfortunately, agreements from institutional background are rarely sent (...) for a prolonged time so, when we receive information of this kind, it (...) has already been modified.” Principals and teachers partially had knowledge regarding the 2010 guidelines. Principals stated they were advised “a few years ago” to reduce food and beverages’ sugar and fat content. Administrative sanctions to the breach of the standards were also unknown. Teachers were worried to be sanctioned, as “it is unfair (…) we are unable to apply something we don’t know”.
Children had up to five opportunities to eat during the school day besides breakfast at home. In chronological order: at the beginning of the school day from street vending, government-subsidized breakfast (available at half of the schools), at recess (brought from home or bought at school vending), during class and from street vending at the end of the school day. Most children (67.7%) ate three to four times while 17.9% ate twice during the school day.
There was no reference or observation of street food vending regulation. Street food vendors were present outside all schools at the beginning and at the end of the school day. Sale of food and beverages included fried snacks, Mexican food preparations (meat-based sandwiches such as tortas or pambazos, and tacos), candy, ice pops, sweetened beverages and plain water. Almost a fifth of the children (18%) bought street food at the beginning of the school day. Food most commonly bought were tortas, followed by sweetened beverages and candy.
A quarter of students (26.1%) often bought street food at the end of the school day. Most frequently purchased products included fried snacks (22.7%), followed by sweetened beverages (22.4%) and plain water (19.7%). Teachers stated parents were not contributing to a healthy lifestyle by giving money to their children to buy food outside the school. One teacher stated that “I do not give them money to buy outside [but] who does that? Parents.”
Healthy environment enhancement was inconsistent. On the one hand, teachers followed the school curriculum by teaching the basis of a healthy diet through the Mexican food guidelines for a proper diet: The Good Eating Plate and The Healthy Drinking Pitcher (El Plato del Bien Comer and La Jarra del Buen Beber). All parents confirmed this topic was covered from preschool. Although parents stated that not all teachers encouraged having breakfast, most children (79%) usually had breakfast at home. Frequency of this practice decreased by school grade: 86% of children in 4th grade, 82% in 5th grade and 70% in 6th grade.
On the other hand, in half of the schools teachers gave children food to sell at recess, and stated that “all schools have school vendings in which children are partners, and for this society to function they have to sell candy”. Besides candy, food included chocolates, prepackaged salted snacks and bottled plain water. This practice was endorsed by principals. One principal stated that it was “part of the education program (…) It comes from many years ago”. The rationale was that children were able to practice basic math and learn to be entrepreneurs. Parents expressed their disapproval of this practice, as children frequently ate the merchandise or lost the money and had to pay the deficit. One parent said children sometimes had to “use their own money; they force you to finish [a batch of products] because (...) there cannot be leftovers”.
Children lacked free access to safe drinking water. All stakeholders confirmed the water from drinking fountains was not suitable for human consumption. As one teacher stated, “water tanks are not clean. It is not alright for them to drink it”. Principals referred the municipal district was in charge of the filter and water tank cleaning. In most cases drinking fountains’ surface was also unclean and contained leftover food or trash, although there was school cleaning staff available.
Most children (88%) did not drink water from school drinking fountains due to lack of hygiene. Of those children who did, most were male (69.2%). A teacher confirmed children consumed it “despite they know they shouldn’t do it”. Bottled plain water was rarely available at school vending, although it was usually bought at street food vending (19.7%) at the end of the school day.
A group of teachers was in charge of the SVC, despite it should only be conformed by parents, as stated in the 2014 guidelines. This was not acknowledged by any of the stakeholders.
Principals, teachers, SVC members and parents reported no formal guidance or training. Members of the SVC expressed their concern as they “have not had access or guidance on how it is carried out, (...) do not know the food, regulations, hygiene norms and anything else”. Nevertheless, they “would like to have those documents to (...) be able to carry out school vending as it should be.”
Food vendors reported a two-hour annual training covering mostly food hygiene. It was conducted by the Ministry of Health (MOH) in the middle of the school year (January). None of the food vendors was aware of the 2014 guidelines’ requirement to include dietitians or dietitian-trained personnel as part of their staff. In most cases, food vendors were students’ parents with no formal food training. A principal confirmed that “until now, there is no counseling for them in food preparation”.
As for nutritional advice, food vendors were told by principals and SVC members to reduce high-fat and sugar ingredients, such as mayonnaise or chili (chamoy) powder or pulp, and to reduce the frequency they offer fried food to once a week or every two weeks. Food vendors expressed their need to be trained in nutrition and food portions. One food vendor stated “they did not explain more like, about calories”; another indicated: “[training] has been so long ago I’ve forgotten”.
Food sale varied by school. Cookies, cake, candy and desserts (CCCD) was the food category most available at schools (36%), followed by vegetables and fruits (25.9%) and food preparations (21.8%). Snacks, which include oilseeds and legumes, were the least offered (16.3%). Food and beverages which were only allowed to be sold on Fridays (according to the 2014 guidelines), were available throughout the week. Furthermore, there was a low level of compliance with SI and SIII of the 2010 (Table 4) and the 2014 guidelines (Table 5).
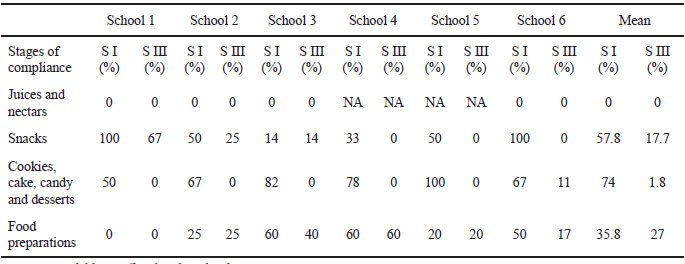
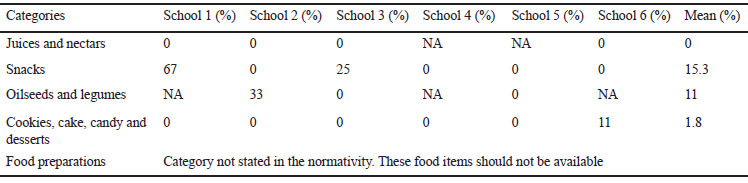
CCCD category partially complied with SI. Compliance was reduced due to excess sugar content. Items mainly included candy, ice pops and commercial cookies. Vegetables and fruits were widely available at all schools. Few items were initially sold with added sugars (e.g. chocolate-covered strawberries, fried banana with condensed milk). However, toppings high in sugar, sodium or fat (e.g. chamoy, chili pulp or powder, salt, sugar, condensed milk, chocolate syrup and jam) were available for children to add without restriction.
Food preparations mostly included Mexican fried traditional dishes. Compliance of this category was low for SI, and decreased in SIII at some schools because of more strict sodium and total fat restrictions. However, none of the items complied with the 2014 guidelines, as the food preparations category was removed. Snacks’ sale included popcorn, corn and prepackaged fried snacks. Compliance varied by school, although two schools met SI 2010 standards. For the rest, energy restriction mainly contributed to low level of compliance in SI. Compliance for SIII and 2014 standards decreased overall due to sodium restriction. For the 2014 guidelines, most oilseeds and legumes sold at schools did not comply because they exceeded energy and sodium limits; these were fried, coated or salted, rather than plain. Finally, juices and nectars at school vending were scarce and didn’t comply with either volume or energy requirements of 2010 or 2014 guidelines. These included Mexican traditional sweetened beverages (aguas frescas) and orange juice.
Almost all children ate at recess (95%). Half the children brought their lunch from home (52.3%), while most children (85.5%) bought food or beverages at school vending. From these, over half of the children (59.6 %) bought one or two items. Food items most usually bought from school vending included tacos (24.6%), ice cream, jelly or flan (19.1%), plain water (15.1%), hotdogs or tortas (11.1%), fruit (10.5%) and juice or lemonade (10.2%). A third (32.6%) of the children received 9 to 12 Mexican pesos (an average of fifty cents USD). Only 10.5% did not receive any money to buy food at the school vending.
SVC members and principals performed food vendors’ recruitment and informal supervision. Each meal offered at school vending was only subject to taste evaluation. Two SVCs relied on a list of recommended foods, allegedly provided by the Ministry of Education (MOE). Half of the schools indicated occasional visits from the MOE’s zone supervisor. However, no supervision was observed. No report was found regarding school food vending performance.
Parents referred they are not informed of what is sold at school; they only observe what food vendors sell when they are present during recess. Nevertheless, they expressed their willingness to receive further information on food sale.
Our study shows low compliance with the Mexican school food guidelines. On paper, school food guidelines follow the World Health Organization (16) recommendations on monitoring food nutritional quality, building a healthy eating environment and staff training. Nevertheless, guidelines’ implementation differed in practice, by a failure on their dissemination, stakeholders’ training and implementation monitoring at schools.
Guidelines were planned to be disseminated in 3 to 4 months, which differs from Canada’s school comprehensive model in which dissemination policy process began four years in advance (17). Low availability and review of the Mexican school guidelines by key stakeholders was previously reported by Théodore (9). This was consistent with the present research, as none of the stakeholders acknowledged the 2014 guidelines, while 2010 guidelines were partially understood. Penalties for nonfulfillment were also unknown and none were applied, although these range from fines (five thousand minimum wages) to revocation of school’s academic validity (7, 18).
Training relied on health and education authorities by both guidelines, but stakeholders differed. At all schools, SVCs only included teachers, who carried out informal supervision of food sale. This was the only well-recognized function of the SVC, as also reported by Théodore (9). As stated on a 2010 guidelines’ review (9), the policy delegated most of its implementation to school stakeholders, without further engagement to ensure implementation. On-site, principals, teachers, members of the SVC and parents expressed a lack of initial and continuous guidance and training, which impeded them from performing their duties appropriately. Although school food vendors lacked enough information, they expressed openness to modify their food products to meet the guidelines’ standards.
A healthy eating environment was not enhanced at schools. In accordance with Bonvecchio-Arenas (5), children had up to five opportunities to eat during the school day besides breakfast at home; hence, food was available throughout the school day. Further research is needed to determine to what extent this contributes to childhood obesity, as most children (67.7%) ate 3 to 4 times during the 4.5 hours of school day. Although two of the five opportunities to eat involved street food vending, and a positive association has been found between the number of street food vendors around schools and children’s BMI (19), no regulation was observed. In line with Shamah-Levy’s findings (20) fried snacks were the most popular street food among children. Regulation and guidance are needed for street food vending to encourage a healthy eating environment, expanding this benefit to the community.
As previous research has shown (4,10), parental nutrition education is also necessary. To convey the importance of breakfast becomes relevant as frequency of this practice decreased by school year. Consistent with Masse and Patino-Fernandez (17,21), most teachers believed it was parents’ responsibility to ensure healthy eating and for them to only cover school curricula. Nevertheless, without proper guidance, this role does not seem feasible for either. As previously reported (21), children’s sale of energy-dense food for fundraising was endorsed in half the schools by principals and teachers. Although fundraising is often used to compensate for school financial issues (17,22), it prevents children from eating properly and participating in physical activity during recess. Thus, fundraising alternatives to food sale must be sought, while school resources’ provision must be ensured by the corresponding authorities.
Compliance with the 2010 and 2014 guidelines was low overall. As expected, it was higher at early stages as standards were less strict, consistent with a previous study by Perez-Ferrer (10). The restrictive SIII and 2014 standards leave out common Mexican foods, making them difficult to follow. Another aspect that influenced compliance was the quantity and quality of the foods offered. Guidelines’ compliance of snacks, oilseeds and legumes would increase if portions were smaller and served plain, rather than salted, coated or fried. CCCDs’ compliance could be enhanced with smaller portions and if high sugar content candy or ice pops were no longer sold. Food preparations, although not allowed by the 2014 guidelines, were highly prevalent. A lower presence of fruits and vegetables was found by Jimenez-Aguilar (8), which differed with the present study since it represented a quarter of the sample (25.9%). However, compliance was limited due to the high availability of toppings high in sugar, fat and sodium.
As previously reported by other studies carried out in Mexican schools, safe drinking water from drinking fountains was not available (5,10). As previously stated by Perez-Ferrer (10), lack of maintenance of water tanks and drinking fountains prevented its use. Logistics for water provision remain uncertain for school stakeholders. Drinking fountains’ infrastructure and maintenance must be clear and ensured, while children must receive education on proper use to ensure hygiene.
Although previous reviews (9, 23) found serious flaws of the 2010 food guidelines: the absence of a legal framework, lack of concrete objectives, goals, time frames and roles, unclear process or coordination mechanisms that translate into straightforward actions, as well as lack of proper indicators to track progress, 2014 guidelines were issued with similar limiting conditions.
In order to enhance acceptance, compliance and adherence, all stakeholders must be involved in the policy from its design. It must include clear goals and indicators. Training, guidance and monitoring are key elements to the guidelines’ implementation, as lack of support, resources and training have been identified as barriers for a healthy environment (24). Additionally, the policy should consider incorporating culturally appropriate eating habits of the Mexican population.
The study has limitations to consider. Normativity modification (from 2010 to 2014 guidelines) at the time of starting data collection (August 2014) compromised the school guidelines’ implementation assessment. Since the new guidelines had three months in force at the time data was collected, it was decided to compare the research findings with both guidelines mainly because all stakeholders were not aware of the normativity changes throughout the whole school year. Likewise, the information obtained can only be generalized to schools in Mexico City with the same sociodemographic characteristics as the participating schools. It is not possible to know the follow-up of the guidelines in public schools located in areas of average socioeconomic level, nor in private schools attended mainly by children of medium-high and high socioeconomic status.
The lack of acknowledgment of the current guidelines due to failed dissemination, undefined roles and policy procedures, absence of training and capacity building for stakeholders hinders school guidelines’ implementation and assessment. As a result, children were subject to an obesogenic environment, with up to five opportunities to eat during the school day, unregulated foods available at recess, limited access to plain water and inadequate support from stakeholders due to lack of capacity building. Compliance with the guidelines was low in all dimensions, although stakeholders were open to guidance and training. A comprehensive approach in which all stakeholders are involved from policy formulation to implementation and assessment is required to achieve the established outcomes. Further research should be focused on the evaluation of the current school food environment across Mexico, and on the assessment of dietary habits of schoolchildren for a longer period of time.
We thank all participants for their time and contribution to the study. The main author deeply appreciates the supportof the National Council of Science and Technology (CONACYT) CVU 481381 for the scholarship provided for her postgraduate studies.
The current research received no specific grant from any funding agency, commercial or nonprofit sectors. There are no conflicts of interest to declare. The content is the responsibility of the authors and does not represent that of any other institution.
Recibido: 28-11-2019
Aceptado: 17-02-2020