 María Fernanda VinuezaVeloz,2,3
María Fernanda VinuezaVeloz,2,3  Carlos Wladimir Palate Supe,4
Carlos Wladimir Palate Supe,4  José Gabriel Carpio Salas,5,6
José Gabriel Carpio Salas,5,6  Yadira Alejandra Morejón Terán,7
Yadira Alejandra Morejón Terán,7  Tannia Valeria Carpio Arias.8
Tannia Valeria Carpio Arias.8 
The reduction of hours of sleep affects the physical and mental health of people. Having unhealthy sleep habits are associated with a greater occurrence of daytime sleepiness, which in turn has been related to poorer nutritional status. The objective of this study was to relate food intake, anthropometric measurements, and daytime sleepiness in Ecuadorian adults. Non-experimental, cross-sectional study, the sample included 400 men and women between 18 and 65 years of age, who attended an outpatient consultation of general medicine, family medicine, and traumatology services of a public hospital in Quito-Ecuador. Anthropometric and body composition measurements were measured using tetrapolar bio-impedance, following the recommendations of the International Society for the Advancement of Anthropometry (ISAK). Caloric intake was measured using a 24-hour recall and for daytime sleepiness (DS) the Epworth questionnaire was used. Statistical analyzes were performed using R. From the sample 56.5% presented DS, which affected women more frequently compared to men (p < 0.05). Differences were found between body measurements and dietary intake between groups of people with and without DS. Caloric intake, waist circumference, percentage of fat mass were higher in people with DS (p < 0.05), while muscle mass was higher in subjects without DS (p <0.05). No differences were found concerning visceral fat. We conclude that SD is related to less healthy values in terms of dietary intake and anthropometric measures. Arch Latinoam Nutr 2021; 71(1): 45-53.
Palabras clave: Cardiovascular risk, corporal composition, daytime sleepiness, nutrition.
La reducción de las horas de sueño afecta la salud física y mental de las personas. Tener hábitos de sueño poco saludables se asocia a una mayor ocurrencia de somnolencia diurna, lo que a su vez se ha relacionado con un peor Estado Nutricional. El objetivo de este estudio fue relacionar la ingesta de alimentos, las medidas antropométricas y la somnolencia diurna en adultos ecuatorianos. Estudio no experimental, transversal n=400 hombres y mujeres entre 18 y 65 años, que acudieron a consulta externa de los servicios de medicina general, medicina familiar y traumatología de un hospital público de Quito, Ecuador tomado como referencia. Se tomaron medidas antropométricas siguiendo las recomendaciones de la Sociedad Internacional para el Avance de la Antropometría (ISAK) y de composición corporal a través de la bioimpedancia tetrapolar. La ingesta calórica se midió mediante un recordatorio de 24 horas y para somnolencia diurna (SD)se utilizó el cuestionario de Epworth. Los análisis estadísticos se realizaron utilizando el software R. 56,5% de la muestra presenta SD, que afectó con mayor frecuencia a las mujeres en comparación con los hombres (p <0,05). Se encontraron diferencias entre las medidas corporales y la ingesta dietética entre grupos de personas con SD y sin ella. La ingesta calórica, la circunferencia de la cintura, el porcentaje de masa grasa fue mayor en personas con SD (p <0.05), mientras que la masa muscular fue mayor en sujetos sin SD (p <0.05). No se encontraron diferencias en relación con la grasa visceral. Concluimos que SD está relacionada con valores menos saludables en cuanto a ingesta dietética y medidas antropométricas. Arch Latinoam Nutr 2021; 71(1): 45-53.
Key words: Riesgo cardiovascular, composición corporal, somnolencia diurna, nutrición.
https://doi.org/10.37527/2021.71.1.005
Autor para la correspondencia: Tannia Valeria Carpio. E-mail: [email protected]
The prevalence of obesity worldwide is alarmingly high with a tendency to increase; as a result, it has been baptized with the term "globesity" (1). Today approximately 2.2 billion people in the world have overweight or obese. Almost 30% of the world's population, and in Latin America about 58% of people live with overweight representing a total of 360 million people (2).
In Ecuador, according to the National Health and Ecuadorians have overweight and 22.2% are obese. This percentage is of concern because obesity is a risk factor of chronic non-communicable diseases such as diabetes, cardiovascular disease (CVD), hypertension, (HT) and various types of cancer, which today represent the main cause of morbidity and mortality in Ecuador (3).
Excessive food consumption as well as a fast transition from traditional food consumption and preparation to westernized food consumption patterns, together with low physical activity are primary factors contributing to obesity. Regular physical activity and maintaining a nutritional balance could serve as a method to prevent overweight, and obesity. In the search for factors associated with overweight malnutrition, it has been described that new aspects such as quality, duration and efficiency of sleep could be part of the etiological factors related to overweight and obesity (4).
Short sleep periods are associated with various hormonal changes including, reduced levels of leptin (appetite suppressant hormone) and increased levels of ghrelin (appetite enhancing hormone), both of which are associated with a higher risk of obesity (5). However, lack of sleep could also be the consequence of normal biological changes (e.g. menopause) and the changing rhythms of modern life, in which individuals are making extensive usage of electronic devices for reading, communication, and entertainment. Such devices emit a blue light that is believed affects sleep by altering the circadian rhythm and promoting poor quality night time sleep as well as increased daytime sleepiness in individuals (6,7).
Previous studies (4,5) suggest that both sleep duration and sleep quality are related to overweight and obesity. While others found that sleep duration in adult people is not related to body weight gain (8,9). Sleep habits could be measured in several ways. Although direct, some of these are less used because they are expensive and complicated to implement (7). An alternative in this way are questionnaires, which are usually easy to use and cheap. One of the parameters that can be evaluated using questionnaires is daytime sleepiness defined as excessive sleep during the day (10). Daytime sleepiness can be measured using the Epworth Daytime Sleepiness Scale, which has been validated for Spanish-speaking people and tested in populations similar to the Ecuadorian (11,12).
The objective of the present work is to study the association between daytime sleepiness, anthropometric measurements, and caloric intake in a group of Ecuadorian adult people.
The research was carried out after complying with the guidelines from the Teaching and Research Department of the “Enrique Garcés General Hospital”. All participants had to sing a written informed consent in order to participate in the study. All data were collected by trained and qualified personnel.
An observational, cross-sectional design was implemented conducted from May 2019 to April 2020. Sample included n=400 men (43.1%, n = 185) and women (56.6%, n = 215) with ages between 18 and 65, who attended the outpatient consultation of three medical services: general medicine, family medicine, and traumatology of “Enrique Garcés General Hospital” Quito, Ecuador. This hospital was selected because it is a public hospital, located in the capital of the country that receives a large number of patients and that authorized the development of this research.
Inclusion criteria were as follows: a) Patients attending the hospital with ages between 18 and 65; b) patients who signed the informed consent form. Exclusion criteria were as follows: a) Women who were pregnant or breastfeeding; b) patients with mobility problems or edema.
Sample size was calculated based on the number of patients treated monthly in the outpatient service of the hospital, the proportion of risk of cardio vascular disease (30%), 2% of error and a 95% confidence interval. An additional 10% was added to the sample in order to take into account possible data loss. Epidat 3.1 program was used to calculate the sample. A final value of 400 patients was obtained.
Anthropometric measurements were taken following ISAK guidelines (13). Weight in kilograms (kg) of each person was obtained using a tetrapolar bio-impedance mechanical scale (OMRON HBF-514C), which has an accuracy of ± 0.1 kg with the minimum amount of clothing and without shoes. Height in centimeters (cm) was evaluated using a stadiometer (Handac) with an 1.0 mm accuracy, locating the plane of Frankfort in the patient. Circumferences of the waist (WC) and hip was measured using a flexible MAAS R tape, rollfix type (Hoechst R) with an accuracy of 1 mm. WC was measured at the narrowest point of the waist. The hip circumference was taken at the maximum point of the gluteal area. Anthropometric measurements were made twice by the same observer with an accuracy of 0.1 kg for body weight, 0.5 cm for height and 1 mm for skin folds; the mean of both values was recorded. Body Mass Index (BMI) was calculated using the following equation, where BMI = weight (kg)/height (m2). BMI was then categorized following WHO guidelines in order to allowed to determinate nutritional status in people between 18-59 years old (14). In this way, nutritional status was classified as follows: <18.5 kg/m2,underweight; 18.5-24.9 kg/m2, normal weight; 25-29.9 kg/m2, overweight; 30-34.9 kg/m2, obesity class I; 35-39.9 kg/m2, obesity class II; >40 kg/m2, obesity class III. In people over 60 years old, normality was considered when BMI was between 22-27 kg/m2. The Waist-Hip Index was calculated using the formula: waist / hip with the following cut-off point: ICC = 0.71-0.85 normal for women. ICC = 0.78-0.94 normal for men. This values are associated with a lower risk of mortality (15).
Cardiometabolic risk was evaluated using various indicators including waist circumference (WC), waist-to-hip index (WHI), and percentage of body fat and visceral fat. For WC in women: <80cm low risk, 80-88cm moderate risk, >88cm high risk. For WC in men: <94cm low risk, 94-102cm moderate risk, >102cm high risk. For WHI in women: <0.75 low risk, 0.75-0.85 moderate risk, >85 high risk. For WHI in men: <0.90 low risk, 0.90-1.00 moderate risk and >1.00 high risk. Percentage of body fat and visceral fat was estimated using tetrapolar bio-impedance with OMRON HBF-514C segmental bioelectric impedance autoanalyzer, which categorize body fat considering age and sex groups in low fat, healthy, high fat and obese. For visceral fat, scores obtained were classified according to cut-off points incorporated in the NHANES (2007): nominal (1-9), high (10-14) and very high (13-30) (16)
Epworth Daytime Sleepiness questionnaire, which was created by Murray Jhons 1991, was applied to subjectively measure daytime sleepiness (17,18). The questionnaire includes eight questions, where the person is presented with situations in which he or she may be sleepy during the day. For the present study we used a questionnaire that was validate in Peruvian population due to similarities in language use (12).
The 24-hour dietary recall was used to assess the caloric intake of participants. It was asked about the consumption in quantity and quality of food the day before, to reduce the brains a photographic album was used to identify the portions of food. For the analysis of the information, the following food composition tables were used: The one of the Institute of Nutrition of Central America and Panama "INCAP" and the Ecuadorian food composition table (19,20).
Descriptive analysis was performed using means and standard deviation, since the variables followed a normal distribution (Kolmogorov-Smirnov p = 0.478). Statistical tests such as T-Test and Chi2 were used for inferential analysis depending on the type of variable. Statistical significance was determined when the test value was <0.05. R and R Studio software was used for statistical analysis (21).
The present study has a duration of a year and a half. Data collection lasted almost a year, due to the need of requesting permits in the city health center.
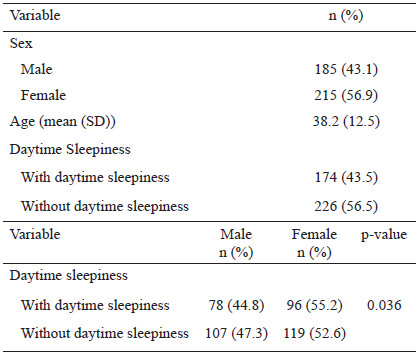
General characteristics by groups: Sample included n=400 men and women (43.1% and 56.9%, respectively). Average age of the sample was 38.2 years (SD 12.5). According to the analysis, people with daytime sleepiness are predominant 56.5%. Female suffer from daytime sleepiness more frequently than male (52.6% vs. 47.3%; p=0.036) (Table 1).
Anthropometric characteristics, caloric intake, cardiometabolic risk and corporal composition of the population: Anthropometric characteristics and caloric intake of the population are summarizing in Table 2. Body weight mean was 67.1kg, being higher for male (72.8 kg) respect for female (62.3 kg) p=0.026. The height means 1.57 m, BMI mean 27.2 kg/m2 being higher for male (31.5 kg/m2) respect for female (26.8 kg/m2) p=0.046 waist circumference means was 96.5 cm (96.0 cm for male and 87.0 cm for female) p=0.018, fat mass mean 33.8% (38.6 for male and 42.4 for female) p=0.039, muscle mass mean 28.6% (31.2% for male and 24.5% for female) p=0.017, and visceral fat mean 8.4% (14.0% for male and 16.0% for female) p=0.059. According to dietary intake, average population consumption was 2986 kcal / day (3377 kcal for male and 2657 kcal for female) p=0.002
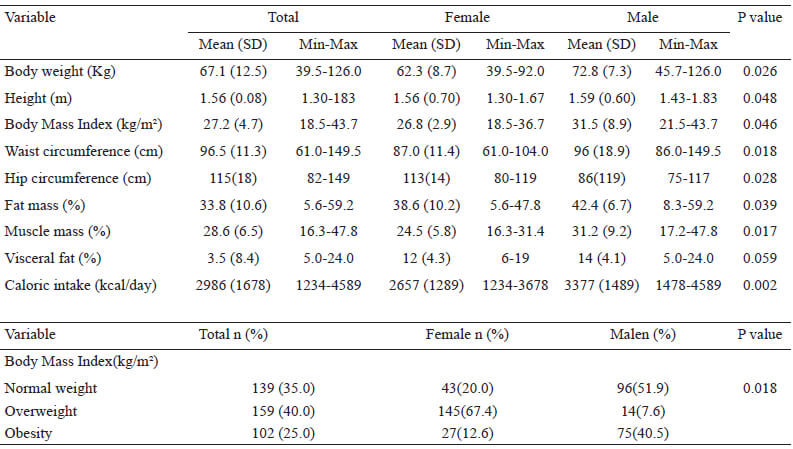
From the sample, 40% were overweight and 25% had obesity. Female presented a higher percentage of overweight (67.4%) compared to male (7.57%) p=0.018.
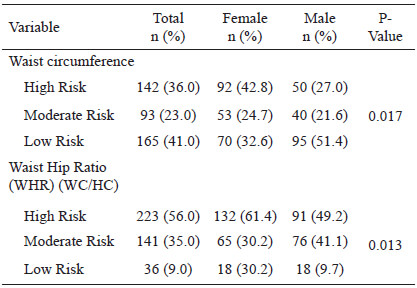
When cardio metabolic risk was assessed by WC, we found that 36% of the sample had high risk, and when people was assessed by WHR this value increased to 56% Cardiovascular risk measured by WHR was higher in women (61.4%) compared to men (49.2%) (Table 3). In addition, a higher percentage was found in female (64.79) compared to male (35.21) with statistically significant differences p = 0.017.
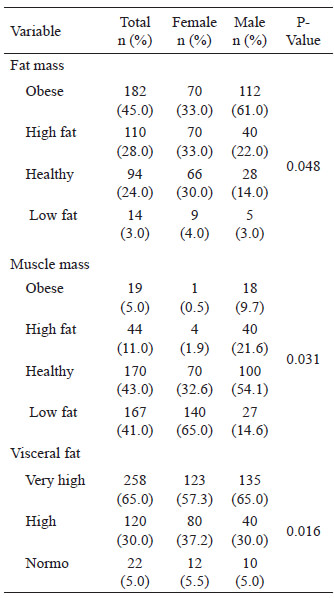
Cardio metabolic risk percentage was consistent with body and visceral fat evaluation. In this way, 45.0% of the sample were obese (61.0% men and 33.0% women) and the 65.0% had very high visceral fat score. Regarding muscle mass amount, the majority (43.0%) were classified as normal and 41.0% with low muscle mass (Table 4). However, the low percentage of muscle mass was lower in female (65.0%) compared to male (14.6%).
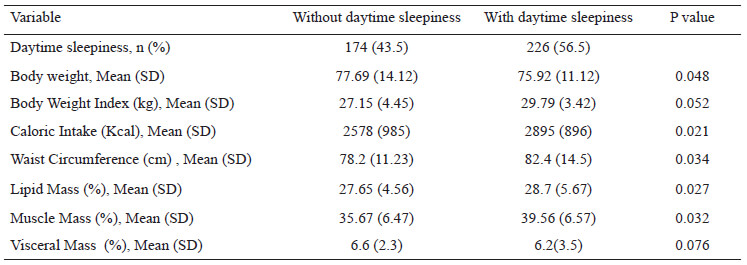
Relation between daytime sleepiness, anthropometric measures and food intake: Analyzes were performed to study the association between daytime sleepiness and anthropometric measures, body composition and food intake. We found differences regarding body measurements and dietary intake between groups with and without daytime sleepiness. In this way, caloric intake (p=0.021), waist circumference (p=0.034), body fat mass percentage (p=0.027) was higher in people with daytime sleepiness comparing with people without. Similarly, muscle mass was higher in people without daytime sleepiness (p=0.032). Regarding the visceral fat mass and body mass index there were no significant differences between the groups (p=0.076 and p=0.052, respectively) (Table 5).
The present study we investigated the association between daytime sleepiness, anthropometric characteristics and caloric intake in adult population of the capital of Ecuador in a sample of 400 adult subjects. Approximately 6% to 45% of the adults have experiences subjective sleepiness, however, in the study was found a 56.5% the daytime sleepiness (22-25) and showed a statistically significant difference in Epworth Daytime Sleepiness (EDS) among males (44.8%) and females (55.2%), p-value = 0.036. The dream has a profound impact on human well-being at multiple levels. The adults need ≥7 h of sleep per night for optimal health and wellbeing (26). In the study by Sa et al., 2020 (27), it was found that obesity was related to both < 7 hours/day and >9 hours/day of sleep, and that poor sleep quality was related to overweight and obesity. So far, no studies have been found that link daytime sleepiness with adiposity indicators as in the present study. The increase the prevalence of obesity is associated changes in lifestyle and environmental factors. Further research is needed to explore the between sleep habits and overweight and obesity (27-30).
There is still controversy on this respect, probably because sleep can be measured in various ways, such as through its duration, efficiency, quality and others (31,32). Likewise, sleep habits are often related to unhealthy habits that can lead to health problems such as chronic degenerative diseases and increase mortality (33). In this way, subjects who sleep less tend to have worse dietary habits, with a higher caloric intake, greater body weight gain (34), lower consumption of fruits and vegetables (35) and less physical activity (36). In the same way, we found a higher caloric intake in people who presented greater daytime sleepiness. Thus, presenting daytime sleepiness as the result of unhealthy sleep habits can be considered as a risk of overweight and obesity.
It should be mentioned that we did not find significant differences regarding BMI in subjects with or without daytime sleepiness. In contrast, other body measurements were associated with daytime sleepiness including, WC and percentage of body fat, both of which are now considered good predictors of cardiovascular risk, diabetes mellitus II and other chronic diseases. In this way, body mass index, although widely used, is a general index of obesity that does not often indicate a person's actual health condition (37).
Although the mechanism of how sleep deficit contributes to weight gain is not well understood, it may be related to changes in satiety and hunger hormones that result in altered food intake. For example, it has been found that sleep problems may be related to energy metabolism and that the body tends to store energy as a response mechanism to lack of sleep (38, 39).
Finally, it is worth mentioning some limitations of this study. For example, one is that the data collected in this study is subjective and depends on the participant's self-assessment. This situation creates the possibility of over reporting or underreporting symptoms, including other associated factors. Other factors such as the use of hypnotic medication, problems such as menopause, the consumption of stimulants such as caffeine should be considered to make a more accurate assessment of the sleep-rest variable.
The present study has a cross-sectional design that was not designed to examine the cause of EDS, which does not allow the establishment of cause-effect relationships. Moreover, a qualitative analysis of food was not carried out to identify whether people could be affected by the consumption of certain foods and include laboratory data, so it is recommended to incorporate these analyses in future research. Additionally, since the included population belong to a specific medical setting, our findings cannot be extrapolated to the general population because the sample is probably not representative. A major advantage of this study compared with other studies is that the association of EDS and adiposity indicator for example visceral adiposity and the differences for sex.
Clinical implications: The results of this study may contribute to a better understanding of overweight and obesity, considering that there are also factors such as sleep habits that should probability considered among lifestyle recommendations to control body weight.
It is concluded, we have confirmed a cross-sectional relationship between daytime sleepiness and adiposity indicators and food intake. This study described the prevalence of EDS by sex and adiposity indicators in adult people. The EDS vary significantly by gender significantly higher in female.
This work is part of the Study entitled "Study of Cardio-Metabolic Risk Factors in Ec-uadorian Adults. EFRICA-EC" approved by the Research Institute of Escuela Superior Politécnica de Chimborazo, who we thank their support and coordination.
The authors declare that they have no conflict of interest.
Recibido: 22/12/2020
Aceptado: 15/04/2021