The objective of this review is to present the impact of nutritional education, physical activity and support network interventions on the nutritional status, cognitive and academic achievement of students under 18 years of age. According to the literature, multicomponent interventions that address diet, physical activity, and involve parents concluded to be more effective in combating obesity and enhancing academic achievement in young people. Therefore, the implementation of public policies that commit to intervene in a timely manner in the first stages of the life cycle, would have a considerably beneficial impact on health. Arch Latinoam Nutr 2021; 71(3): 228-235.
Keywords: academic achievement, nutritional intervention, nutritional education, childhood obesity.
El objetivo de esta revisión es dar a conocer el impacto de las intervenciones de educación nutricional, actividad física y redes de apoyo en el estado nutricional, rendimiento cognitivo y académico de estudiantes menores de 18 años. De acuerdo con la literatura, las intervenciones de carácter multicomponente que abordan alimentación, actividad física, e involucran a los padres concluyeron ser más efectivas para combatir la obesidad y potenciar el rendimiento académico en jóvenes. Por lo tanto, la implementación de políticas públicas que permitan intervenir de forma oportuna las primeras etapas del ciclo vital, tendrían un impacto considerablemente beneficioso para la salud. Arch Latinoam Nutr 2021; 71(3): 228-235.
Palabras clave: rendimiento académico, intervención nutricional, educación nutricional, obesidad infantil.
https://doi.org/10.37527/2021.71.3.007
Autor para la correspondencia: Sharon Viscardi, E-mail: [email protected]
The 5% of the global population present excess malnutrition, this means that are approximately 115.1 million children with obesity worldwide, thus turning the prevalence of excess malnutrition in a growing worldwide concern (1,2). Chile has positioned itself as one of the countries with the highest rates of obesity, with 24.6% in children aged 6 to 7 years and 31.2% in the population over 15 years (3). The severity of the problem may be more notable among socioeconomically vulnerable children, among which the prevalence of excess malnutrition is almost twice that of their counterparts (4). The causes of obesity are variable and often interconnected (5), with studies attributing it to lack of physical exercise, genetic predisposition, high caloric intake, and mental disorders (6). Many factors that contribute to obesity can be targeted by interventions. However, an understanding of where these interventions are needed and whether or not they are successful is essential for effective policy implementation (5). Studies indicate that schools are the ideal setting in which people can acquire healthy habits throughout their formative years (7). In this context Schools become a crucial environment for the implementation of obesity prevention interventions aimed at improving eating behavior, increasing levels of physical activity (PA), reducing sedentary behaviors, and seeking methods and techniques to include parents in order to achieve greater adherence of children to the different programs (8). This have a main importance since overweight and obesity at this stage of the life cycle are not only associated with immediate health risks but can also progress into adulthood, leading to the development of a series of chronic non-transmissible diseases. In Chile, a review revealed that childhood obesity has been negatively associated with the structure and function of various brain regions that underlie cognitive processes (9), impairing academic achievement during childhood (10,11). However, studies indicate that a balanced diet, an adequate number of hours of sleep, a reduction in screen time and PA have been associated with better academic achievement, cognitive functioning and brain morphology in children (10). In line with the above, the objective of this report is to disseminate the available evidence regarding interventions related to nutrition education, physical activity and support networks and their effect on the nutritional status, cognitive and academic achievement of children.
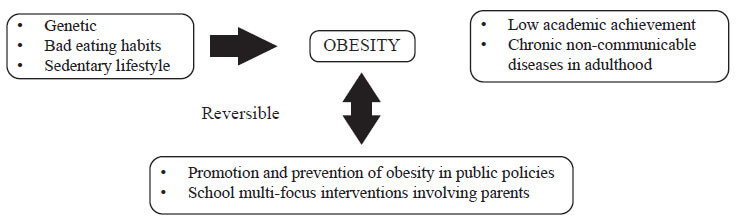
Malnutrition by excess is a complex condition that in the long term can have an impact on the neurological health of people (12), being associated with a greater risk of accelerated cognitive deterioration (13) due to a decrease in cerebral blood flow in the prefrontal regions involved in attention, reasoning, and executive function (14). In addition, obesity is associated with a reduced volume of gray matter (10, 14, 15, 16) as well as with an impaired white matter microstructure, due to inflammation generated by pro-inflammatory cytokines resulting from the accumulation of adipose tissue (12). It is important to bear in mind that structural alterations of the brain might not be the cause but rather the consequence of obesity (17), and they could be negatively associated with cognitive control and academic achievement during childhood (10) (11). In this context, we have to take into account that obesity-related behaviors such as increased intake, disinhibited eating, sedentary activity, and lower physical activity are generally related to greater executive dysfunction, poorer motor skill, and lower academic achievement (18,19). Three healthy lifestyles such as a balanced diet, enough sleep and low screen time are reported to be found in the high performance group for academic grades (11). Moreover, it is reported that a high BMI is negatively associated with peer acceptance and academic achievement, while peer acceptance is positively associated with academic achievement (20). Even if we do not have information regarding the alterations suffered by the brain in the early stages of the life cycle associated with overweight and obesity, we know that these changes are reported in the literature in adults, and on the other hand we know that there is an association between obesity and lower academic achievement in children. For this reason, this should be a point of discussion for the scientific community.
Higher levels of physical fitness (i.e., cardiorespiratory fitness, speed-agility, and muscle fitness) have been associated with better academic achievement, cognitive functioning, and brain morphology in previous studies in children (10, 11). A multidisciplinary treatment program, combining diet, cognitive-behavioral therapy, and physical activity, led to an increase in the volume of the cerebellum and total gray matter in children with obesity, and the observed changes in gray matter volume could be the basis for different cellular and molecular biological mechanisms such as axonal sprouting, synaptogenesis, neurogenesis, gliogenesis and/or vascular changes (16). In contrast, evidence regarding the beneficial effect of PA interventions on overall cognitive and academic achievement in children has proven to be inconclusive, showing a positive change only in mathematics (21, 22), while no changes are reported in executive functioning (16). However, although there is evidence in contrast and still preliminary regarding the positive effect in terms of academic achievement of interventions focused on physical activity, it would be important to create a discussion on the importance of interventions aimed at combating obesity, with a comprehensive perspective. Which would probably allow direct benefits (healthy habits, reduction of childhood obesity) and indirect benefits (better academic achievement).
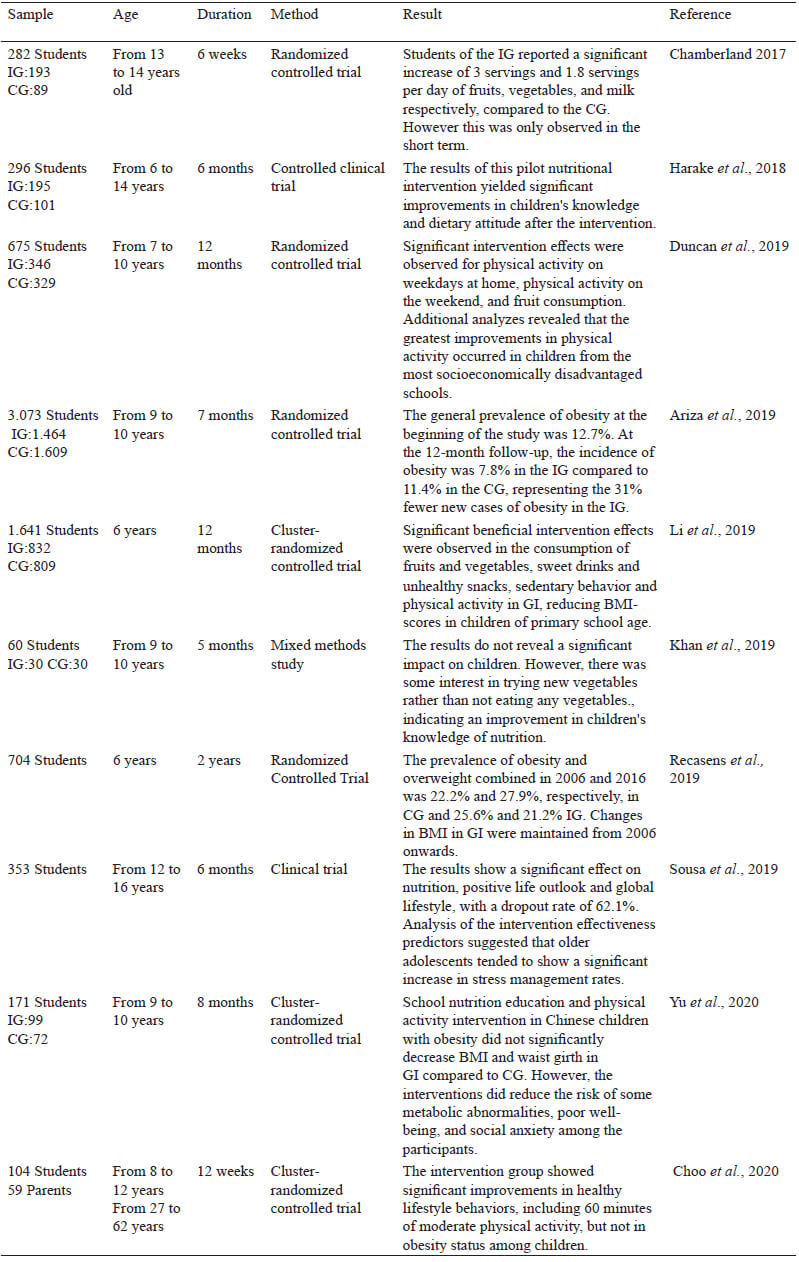
School is the place where children spend half their waking hours and consume at least a third of their daily calories (23), therefore it offers a key opportunity to implement early health promotion programs (8, 24, 25, 26) aimed at generating an effective change in the family environment (20). It has been shown that health promotion programs in schools consistently have a positive impact on knowledge related to nutrition, healthy food selection during school meals, nutrition self-efficacy, and willingness to try fruit and vegetables (27). On the other hand, for school-age children, the family environment is key to achieving successful and sustainable interventions. Parents play an influential role in promoting healthy dietary and PA behaviors in children (4, 24, 28), not only through parenting practices and rules, but also by providing a supportive environment for these behaviors and serving as positive role models (28), encouraging children to try new foods and imitate the healthy eating behavior of their parents (24). The literature suggests that programs that include parental involvement are essential for the prevention of childhood obesity (29) and are more likely to produce better results in the child's weight (26, 30, 31). It is important to notice that, since unhealthy dietary habits and physical inactivity are the main drivers of weight gain, they represent key targets for obesity prevention and treatment interventions (32), with multicomponent interventions addressing both diet and PA presenting more promising results for combating obesity (8, 16, 26, 33, 34). In this context, there is evidence that multicomponent interventions have been successful in promoting healthy eating habits and physical activity in children (5, 35). For example, a multicomponent obesity intervention school program carried out in Barcelona achieved a reduction in the incidence of obesity, stating that it could prevent 1 out of 3 new cases of obesity in children aged 9 to 10 years (36). Another multicomponent intervention program revealed that children in the intervention group, compared to those of the control group, showed significant improvements in levels of knowledge, healthy lifestyle behaviors, specifically unique behaviors such as vegetable consumption and days of sufficient activity, although it did not produce a significant effect on childhood obesity (4). A study of nutrition education intervention and PA that evaluated metabolic parameters indicated that the intervention group achieved improvements in well-being, exhibited lower social anxiety, decreased diastolic blood pressure and fasting plasma glucose, and significantly increased plasma high density lipoprotein from the beginning to the end of the intervention (34). We could conclude that when we think about an intervention implementation we have to focused on all the key targets for obesity prevention and involve parents and school.
Contemporary society has undergone various transformations from a technological point of view, and currently people have greater access to computer resources. The use of the Internet is considered a potential educational and preventive tool in the area of health (37), making traditional space barriers disappear and, in this case, providing greater access to nutritional care through socalled “tele-nutrition”, i.e. the provision of evidence-based medical nutrition therapy by a nutritionist using interactive electronic information and telecommunications technology such as videoconferencing with patients in a remote setting (38). Studies indicate that adolescents who use computer-adapted interventions respond better to personal motivational factors that influence behavior (37, 38). In the covid-19 pandemic context, tele-nutrition seems to be an important strategy to accompany patients, and guided strategies are being developed to achieve anthropometric evaluation in remote (39). Furthermore, the tele-nutrition interventions can be carried out in combination with other actions and compose a set of comprehensive health education programs (37). It was identified that online nutrition education interventions are more likely to be effective when they include personalized messages and/or comments, thus offering regular interaction between participants and researchers and making it possible to establish the appropriate duration of the intervention (40). It is also reported that online interventions can be successful in achieving a change in dietary behavior in a variety of populations, with improvements observed in 14 of 19 reported interventions (37, 38, 40). A study on an online course mentioned that its participants adopted general changes in eating habits for themselves and their families, consuming a greater variety of foods and modifying portion sizes. As a result of taking the course the 54% of students stated that they were considering future studies in nutrition, while the other 46% stated that they did not learn anything new and that the information was too basic (41). Other studies indicate that when nutrition education is visualized and multimedia techniques are used to facilitate understanding of the content, there is a greater effect on fiber intake in both the short and long term, as well as a marginal short-term improvement in the consumption of fruits and vegetables (30, 42). The scientific evidence suggests us that involve technology can be an important part of the intervention, but we believe that the duration of tele-nutrition video capsules must take into account that weight gain is related to sedentary behavior. So, when we ask children, as part of the intervention, to learn about healthy food intake by watching videos, we cannot advise them to sit for a long time, which increases the amount of sedentary behavior and could lead to weight gain. For this reason, the interventions video capsules have to be brief and must propose dynamic activities to practice the acquired knowledge.
It has been shown that childhood obesity is not only reflected in chronic non-communicable diseases, but also affects the brain, generating a negative impact on a structural level, causing progressive cognitive deterioration and consequently lower academic performance. This is the reason why Public policies that allow timely action in the early stages of the life cycle must be urgently implemented to reduce the alarming figures of excess malnutrition, through the development of strategies for the promotion and prevention of obesity, research of new methods interventions, such as online nutritional care, examine how users participate in the interventions and, therefore, which behavior change techniques are most effective, also emphasize the implementation of multi-component interventions for the prevention of malnutrition due to excess and evaluate the impact and effectiveness of these.
This work was support by project grant number VIP-UCT-412-4447 funded by Universidad Católica de Temuco, Chile.
Authors have no conflicts of interest to disclose.
Recibido: 29/06/2021
Aceptado: 20/08/2021