Introduction: At present, education in Health Sciences requires interaction with real patients, which is made more complex due to the need to ensure their health safety. For this reason, new teaching methodologies are now being implemented, which help to improve and protect safe care. Objective: This study was carried out using a quantitative approach with a non-experimental, descriptive design. Materials and Methods: The sample was non-probabilistic and consisted of 87 undergraduate students. A questionnaire was used, with 18 statements divided into 3 dimensions: dimension 1, simulation structure, with six questions reflecting aspects related to its implementation; dimension 2, learning, with seven questions related to aspects of effective communication, trust, learning and respect for diversity; dimension 3, feedback for learning, with five questions, including feedback by the teacher and the simulated patient, as well as their own views with regard to participating in another similar experience again. A five-point Likert scale was used. Results: The three dimensions studied, simulation structure, learning and feedback for learning, report a high level of positive perceptions. Conclusion: The simulation strategy is an educational tool in health-related careers that enhances the clinical competencies of the students as well as the relevant theoretical and practical skills and abilities in their learning process, promoting integration of the knowledge acquired in previous subjects. Arch Latinoam Nutr 2022; 72(2): 93-99.
Key words: clinical simulation, teaching methodology, learning activities, undergraduate students, Nutrition and Diethetics.
Introducción: En la actualidad, la formación en Ciencias de la Salud requiere de la interacción con pacientes reales, lo que se hace más complejo por la necesidad de velar por la seguridad de su salud. Por ello, ahora se están implementando nuevas metodologías docentes que ayudan a mejorar y proteger la atención segura. Objetivo: Este estudio se llevó a cabo con un enfoque cuantitativo con un diseño no experimental, descriptivo. Materiales y métodos: La muestra fue no probabilística a conveniencia y estuvo conformada por 87 estudiantes de pregrado. Se utilizó un cuestionario, con 18 enunciados divididos en 3 dimensiones: dimensión 1, estructura de simulación, con seis preguntas que reflejan aspectos relacionados con su implementación; la dimensión 2, aprendizaje, con siete preguntas relacionadas con aspectos de comunicación efectiva, confianza, aprendizaje y respeto a la diversidad; dimensión 3, retroalimentación para el aprendizaje, con cinco preguntas, que incluye la retroalimentación del docente y del paciente simulado, así como sus propias opiniones con respecto a participar nuevamente en otra experiencia similar. Se utilizó una escala tipo Likert de cinco puntos. Resultados: Las tres dimensiones estudiadas, estructura de simulación, aprendizaje y retroalimentación para el aprendizaje, reportan un alto nivel de percepciones positivas. Conclusión: La estrategia de simulación es una herramienta educativa en carreras afines a la salud que potencia las competencias clínicas de los estudiantes, así como las destrezas y habilidades teóricas y prácticas pertinentes en su proceso de aprendizaje, favoreciendo la integración de los conocimientos adquiridos en materias anteriores. Arch Latinoam Nutr 2022; 72(2): 93-99.
Palabras clave: simulación clínica, metodología de la enseñanza, actividades de aprendizaje, estudiantes de pregrado, Nutrición y Dietética.
https://doi.org/10.37527/2022.72.2.003
Autor para la correspondencia: Sharon Viscardi PhD, Professor, E-mail: [email protected]
At present, education in Health Sciences requires interaction with real patients, which is made more complex due to the need to ensure their health safety. For this reason, new teaching methodologies are now being implemented, which help to improve and protect safe care (1,2).
This requires a different way of teaching, where professionals develop critical and reflective thinking and skills that allow them to face different clinical situations while protecting the safety of their patients. In other words, a change in learning strategies, given that, as the article points out, educational models based on the acquisition and development of skills began to be applied in Latin America in the early 2000s (3,4).
The International Institute for Higher Education in Latin America and the Caribbean (IESALC), in 2006, released "The Metamorphosis of Higher Education", a document that shows the main transformations and challenges of higher education, highlighting the need to analyze the training processes that are developed in universities (5). In relation to the above, universities in Latin America, concluded that it was necessary to move toward a curriculum based on competencies (5,6), setting aside traditional class lecturing in favor of approaches incorporating more collaborative, dynamic and personalized learning (7,8).
Working under a competency model puts students at the center and teaches them to develop skills and aptitudes corresponding to their disciplinary work, allowing them to integrate different types of knowledge and learning that bring them as close as possible to the real life context (5). This encourages putting into practice new teaching-learning styles, where not only knowledge is reflected, but also the skills and abilities grouped into competencies that students must acquire to complete their learning process (9).
Clinical simulation is an interactive learning method that replicates real-life situations (10,11). This allows the development of skills and qualities, integrating theoretical and practical knowledge (12,13) as well as human factors, enhancing clinical skills, and where the student is able to face challenging situations in a safe environment, including the possibility of making mistakes, visualizing the mistake and looking for new learning opportunities (14).
The incorporation of simulated clinical practice can be developed in various ways, one of which is role playing. This can be defined as a theatrical representation of a real situation, where there is a simulated or standardized patient, who is an actor trained to play an active role, representing a real story in a simulated context, thus allowing the student to put into practice the theoretical knowledge learned and explore the vulnerability of the patient in a safe space (15). This methodology, applied and supervised by the teaching teams, favors self-learning and autonomous work within the same simulation context (16).
In Chile, clinical simulation is used as a teaching-learning methodology in the training of health professionals, preferably in careers such as medicine and nursing, but it is incipient in nutrition and dietetics careers, representing a potential tool for student learning. It is therefore relevant to learn how those students perceive the use of this tool.
The Universidad Católica de Temuco (UCT) has put into action an educational model based on competencies, adjusted to the current requirements of higher education (17). In this way, the Nutrition and Dietetics career has implemented clinical simulation with dramatization in two subjects of the curriculum (Evaluation of Nutritional Status and Nutritional Care in the Life Cycle) and is used as an innovative student-centered teaching strategy.
Hypotheses. The perception of undergraduate students of Nutrition and Dietetics regarding clinical simulation with dramatization is positive learning strategy and the simulation will be a good educational paradigm based on the acquisition of competences.
This study was carried out during one year using a quantitative approach with a non-experimental, descriptive design (1). The sample was non-probabilistic for convenience and consisted of 87 undergraduate students.
A questionnaire was used, with 18 statements divided into 3 dimensions: dimension 1, simulation structure, with six questions reflecting aspects related to its implementation; dimension 2, learning, with seven questions related to aspects of effective communication, trust, learning and respect for diversity; dimension 3, feedback for learning, with five questions, including feedback by the teacher and the simulated patient, as well as their own views with regard to participating in another similar experience again. A five-point Likert scale was used (ranging from 5= Strongly agree to 1 = Strongly disagree). The sum of the points attributed to each item defined the total score, ranging from 18 to 90 points. This questionnaire was designed and applied by the researchers, and its content validity was tested by means of the Delphi method (18).
This study was approved by Research Ethic Committee of Universidad Católica de Temuco Chile. Voluntary and informed participation was considered, together with the protection of personal data through the codification of the students’ identities. Participants were informed that they could withdraw from the study at any time.
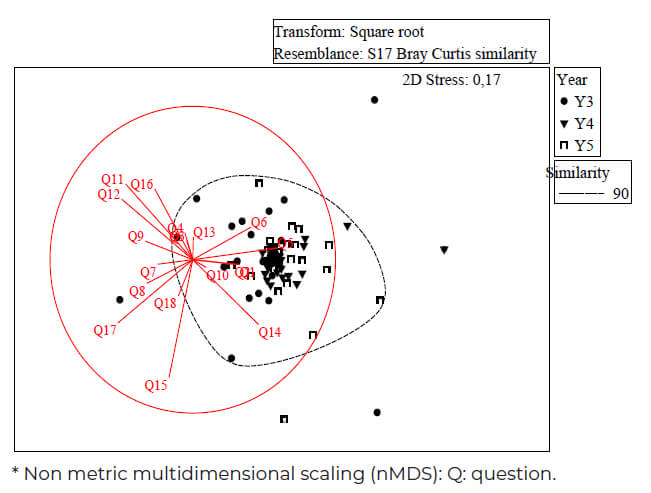
To determine differences (p < 0.05) between the variables analyzed (gender, university career year and previous experience in simulation) based on observed responses, the following was conducted Kruskal–Wallis test followed by Dunn’s post-hoc test, the analysis was carried out with R software. A Non metric multidimensional scaling (nMDS) analysis was performed to visualize the pattern of responses observed for the different generations based on the set of questions studied calculated from the Bray Curtis similarity matrix, the software PRIMER v6 (PRIMER-E Ltd.) were used for nMDS data analysis.
The sample was non-probabilistic and consisted of 86 undergraduate students, made up of 74 women (86%) and 12 men (14%). A convenience sampling method was used and the participants were accessed through the teachers of the courses.
The age of the participants ranged between 20-24 years, (69%) and 25-30 years, (31%). All students of the Nutrition and Dietetics career at UC Temuco who were currently enrolled in the subject of Nutritional Assessment (4th semester) or Nutritional Care in the Life Cycle (8th semester), were asked whether they would like to participate voluntarily in the study.
Table 1 shows the central tendency values obtained by the students regarding the variables gender, year of career and prior experience in the use of clinical simulation in any subject, in each of the indicated dimensions. In turn, Table 2 shows that in the three dimensions studied (simulation structure, learning and feedback for learning) high percentages of positive perceptions
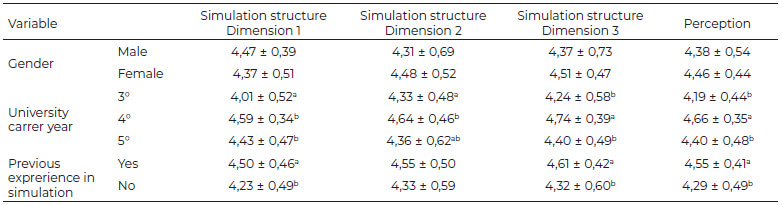
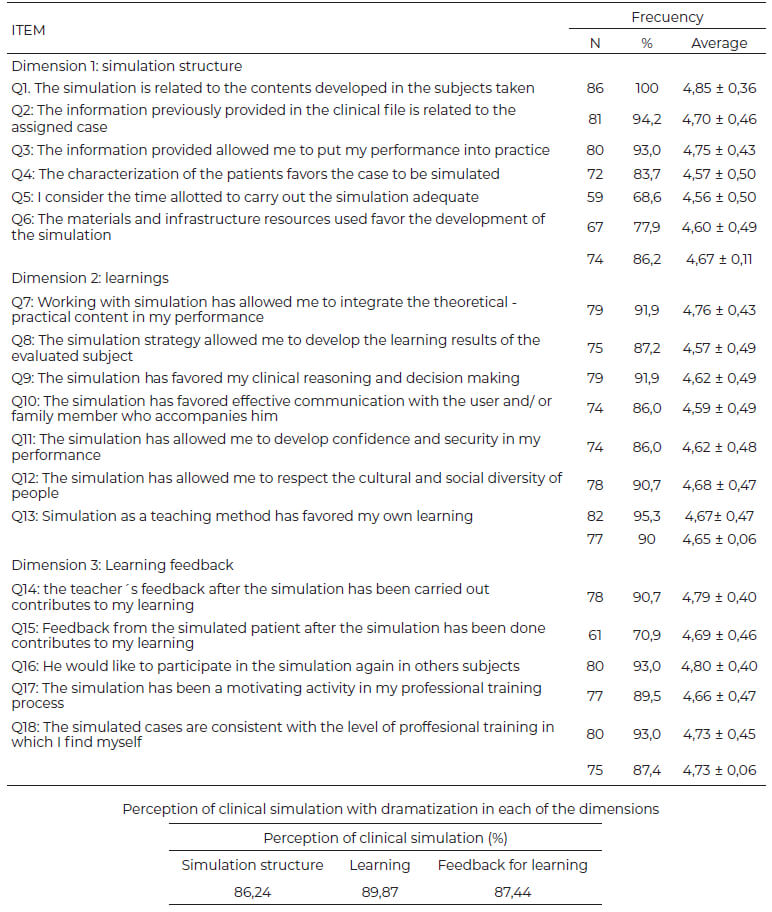
(86,2 %, 89,9 % and 87,4 %) were reported by the participants in relation to clinical simulation with dramatization as a teaching strategy. The percentages were obtained from the application of a Likert scale, where the students were asked to fill in a questionnaire encompassing the above-mentioned three dimensions and were given a 20-minute deadline to respond. In the non-metric multidimensional scaling (nMDS, Figure 1) a high similarity in the response pattern is evidenced with a stress value <0.2 (good representation in reduced dimensions), this pattern of student responses presents between 87-90% of similarity, among the generations analyzed in this study there is a 10% dissimilarity, which raises a cross-sectional system of questions compared to a group of students from different generations. According to figure 1, a high correlation is observed between the observed response patterns and the evaluated questions (Pearson's correlation <0.2), questions of dimension 1 such as Q1, Q5, Q6 are strongly correlated with the observed response pattern. among students of the 3 generations.
The three dimensions studied in this study, simulation structure, learning and feedback for learning, report a high level of positive perceptions which reflects that the simulation strategy is an educational tool in health-related careers that enhances the clinical competencies of the students as well as the relevant theoretical and practical skills and abilities in their learning process, promoting integration of the knowledge acquired in previous subjects (6).
This finding is corroborated by different international educational entities, showing that clinical simulation in the training of health professionals has a positive impact as a teaching-learning methodology (19).
Working on the dramatization with a standardized patient facilitates the teaching process by enhancing clinical reasoning and decision-making in different clinical situations, where the student gets to interact with the patient, focusing not only on the procedure but also on establishing a relationship with him/her. This contributes to the confidence that learners develop when facing a real user (9,19). As proposed by Harder (20), simulation significantly improves patient safety.
This strategy allows immediate feedback from the teacher, which is well accepted by students since it allows them to correct mistakes and to improve and reinforce the skills, abilities and knowledge acquired, and this is consistent with what was noted in the research of Ávila et al. (19).
As Moya et al. (21) suggest, clinical simulation as a teaching methodology can contribute to the training of health science professionals, affording students a closer view of reality as well as bolstering their self-confidence while ensuring patient safety, thus significantly improving their perception of this methodology. As stated by Harder (20), simulation has proven to be effective in enhancing safety competencies in the different disciplines
As similarly proposed by Zambrano (13), this strategy makes it possible to integrate theoretical and practical concepts through the deployment of skills and qualities.
It is an important part of the process to have controlled and safe simulated scenarios, as close to reality as possible, allowing students to make mistakes and learn from those mistakes, focusing on their self-reflection and self-evaluation for their own learning.
Our results are consistent with the various studies regarding the evaluation of clinical simulation as a teaching method, together with what is expected from its development in the enrichment of skills, knowledge, techniques and good performance.
Continual evaluation of the direct participants and their views regarding the method is essential for the improvement of the model and its contribution to the training process (14,22), and should include asking them their opinion on a regular basis.
It is also relevant to deepen the students' perception regarding clinical simulation in order to identify opportunities and improvements in the strategy, thus enriching the learning process.
In this study the undergraduate students of Nutrition and Dietetics found that the clinical simulation with dramatization was a positive learning strategy. The results obtained are a valuable contribution to the training of students in the health sciences, especially in the nutrition career, where clinical simulation is used today, but in an incipient way. Our results demonstrated that the simulation will be a good educational paradigm based on the acquisition of competences.
This work was support by project grant number VIPUCT2019PRO-SV-05 funded by Universidad Católica de Temuco Chile.
Authors have no conflicts of interest to disclose.
Recibido: 05/03/2022
Aceptado: 05/05/2022