 ,
Maria Luiza Amorim Sena Pereira1,2
,
Maria Luiza Amorim Sena Pereira1,2  ,
Bruno Klecius Andrade Teles1,2
,
Bruno Klecius Andrade Teles1,2  ,
Débora Borges dos Santos Pereira3
,
Débora Borges dos Santos Pereira3  ,
Glaucia Cristina de Campos1
,
Glaucia Cristina de Campos1  ,
Maria del Carmen Bisi Molina1,4
,
Maria del Carmen Bisi Molina1,4 
Introduction: Food insecurity (FI) is a state characterized by instability and irregularity of access to food. This condition has negative impacts on dietary intake, affecting nutritional status and health condition. Objective: To evaluate the association between malnutrition and FI among communitydwelling older adults attended to under the Family Health Strategy (FHS). Materials and methods: This is a cross-sectional study conducted using communitydwelling older adults attended to under the FHS in the municipality of Barreiras, in Bahia, Brazil. Between 2017 e 2018, we collected demographic, social, economic, health condition, lifestyle, anthropometric, and food consumption data. We evaluated nutritional status using the Mini Nutritional Assessment (MNA) and we assessed FI with the Brazilian Food Insecurity Scale (EBIA). Besides the chi-squared test, we carried out a binary logistic regression to verify the association between malnutrition and FI, adjusted for possible confounding factors. The significance level was p<0.05. Results: We evaluated 307 older adults with a mean age of 70.4 (±7.5 years). The prevalence of malnutrition/risk of malnutrition was 35.2% and that of FI was 63.5%. Households with older adults in moderate/severe FI presented almost three times more chance (OR 2.97; CI95% 1.37-6.44) of having malnutrition compared with those in food security. Conclusions: The study indicates that there is an association between household FI and malnutrition/risk of malnutrition among older adults from the FHS, especially among those in severe FI. This result attributes to FI the status of determinant of malnutrition in older adults within the context investigated. Arch Latinoam Nutr 2022; 72(4): 274-284.
Keywords: older adults, food insecurity, nutritional status, malnutrition, family health.
Introducción: La inseguridad alimentaria (IA) es un estado caracterizado por la inestabilidad e irregularidad en el acceso a los alimentos. Esta condición tiene impactos negativos en la ingesta de alimentos, afectando el estado nutricional y la condición de salud. Objetivo: Evaluar la asociación entre desnutrición e IA en adultos mayores comunitarios atendidos en la Estrategia Salud de la Familia (ESF). Materiales y métodos: Estudio transversal realizado con ancianos de comunidad atendidos en la ESF del municipio Barreiras, Bahía, Brasil. Entre 2017 y 2018, se recolectaron datos demográficos, sociales, económicos, condición de salud, estilo de vida, antropométricos y de consumo de alimentos. El estado nutricional se evaluó por la Mini Evaluación Nutricional (MEN) y la IA con la Escala Brasilera de Inseguridad Alimentaria (EBIA). Además de la prueba de chi-cuadrado, se realizó una regresión logística binaria para verificar la asociación entre desnutrición e IA, ajustada para posibles factores de confusión. El nivel de significancia fue p<0,05. Resultados: Fueron evaluados 307 ancianos, con una edad media de 70,4 (±7,5 años). La prevalencia de desnutrición/riesgo de desnutrición fue de 35,2% y la de IA de 63,5%. Los hogares con adultos mayores en IA moderada/grave presentaron casi tres veces más chance (OR 2,97; IC95% 1,37-6,44) de tener desnutrición en comparación con aquellos en Seguridad Alimentaria y Nutricional. Conclusiones: El estudio apunta que existe asociación entre la IA domiciliaria y desnutrición/ riesgo de desnutrición entre los ancianos de la ESF, especialmente entre aquellos con IA severa. Este resultado atribuye a la IA un estatus de determinante de la desnutrición en ancianos en el contexto investigado. Arch Latinoam Nutr 2022; 72(4): 274-284.
Palabras clave: anciano, inseguridad alimentaria, estado nutricional, desnutrición, salud de la familia.
https://doi.org/10.37527/2022.72.4.005
Autor para la correspondencia: Marlus Henrique Queiroz Pereira, E-mail: [email protected]
An adequate nutritional status (NS) is fundamental in the aging process, helping to maintain good health and reducing the risk of morbidities (1,2). The elderly population, however, is exposed to alterations in NS, such as obesity, sarcopenia, malnutrition, and cachexia (3,4). Among these, malnutrition is still considered a public health problem, related with the appearance of health issues, chronic and degenerative diseases, and increased mortality (5). One of the aspects related with malnutrition in older adults is food insecurity (FI), a condition that limits and conditions food consumption, compromising the NS of these individuals (6,7).
With the aging process, the body undergoes physiopathological alterations that can contribute to a reduction in dietary intake, as well as unintentional weight change (4,5). Among the determinants of malnutrition in older adults, we can mention alterations of the digestive system, reduced sensorial function, the use of multiple medications, loneliness, depression, consumptive diseases, and functional and cognitive decline, which compromise the older adult’s capacity to acquire, prepare, and consume foods (5,8). Besides these aspects, FI, which is characterized by physical and economic difficulties in accessing foods, can represent another important predictor of malnutrition, especially by producing alterations in food consumption among older adults exposed to this condition (6,9).
Dietary strategies created by older adults in FI include reducing the quantity of foods consumed, as well as decreasing diet quality, causing a reduction in the general quantity of macro and micronutrients ingested (7,10). Consequently, these individuals can become more exposed to malnutrition, nutritional deficiencies, and a more compromised general state of health (11–13).
The Family Health Strategy (FHS) is a nonmaterial technological innovation in health, derived from a more comprehensive conception of the health-disease process, ensuring a powerful and effective approach to organizing Primary Health Care (PHC) in Brazil, with a very important impact on the health of the Brazilian population (14,15). Despite community-dwelling older adults cared for through the FHS having a certain degree of social protection through access to periodic medical consultations, diagnostic testing, free medications, and the possibility of referrals for specialist treatments, these people generally present a lower socioeconomic level and a higher degree of vulnerability, thus being more exposed (to the factors related) to malnutrition and FI (16-20).
Given the scarcity of studies on this topic (7), the increase in FI, and the permanence of malnutrition as a serious nutritional disorder among older adults, it is important to understand the relationship between these conditions, especially when there is evidence that FI and its different forms (mild, moderate, and severe) influence the appearance of malnutrition. Thus, the aim of this study was to evaluate the association between malnutrition and FI among communitydwelling older adults attended to under the FHS.
This is a cross-sectional and quantitative study
conducted using older adults living in private
households, linked to a parent project entitled
“Health assessment of older adults in the municipality
of Barreiras (BA).” The city of Barreiras is located in
the west of Bahia, in the Northeast region of Brazil,
and has an estimated population of 158 thousand
inhabitants (21). It is notable for its agricultural sector
and has a high human development index (HDI)
(0.721). However, in 2021, 7% of the population were
living in poverty and 19% in extreme poverty ( The target population of this study was formed of
community-dwelling older adults (≥60 years old)
attended to under the FHS, a PHC program of the
Unified Health System (SUS). In 2018, the coverage of
the FHS in Barreiras was 52.5%, resulting in a public
of 4828 older adults registered at Family Health Units
(FHUs). The sample calculation of the parent project,
which featured multiple objectives and outcomes,
considered a general prevalence of 50%, a 5% error,
and a 95% confidence level, leading to a total sample
of 356 participants. Considering that the original sample was not
estimated to investigate the object adopted in this
study, we chose to calculate the power of the study
a posteriori, using the OpenEpi software (OpenEpi, Atlanta, Georgia). The sample of older adults enabled
us to identify an odds ratio (OR) of 2.8, considering a
98% test power, 5% significance level, 44% prevalence
in those exposed, and 20% prevalence in the nonexposed. The sample selection took place in two stages. First,
we carried out stratified random sampling with
proportional allocation, where we ran a calculation
considering the 23 territories covered by the FHS
teams to determine the quantity of older adults in each
stratum, in order to guarantee the representativeness
of the sample. Subsequently, based on the proportional
quantitative calculation and the nominal list of older
adults in the teams, we carried out simple random
sampling to choose the older adults in each team. We included in the study older adults aged 60 or older,
of both sexes, who were urban dwellers and registered
at the FHUs. We excluded older adults who were
institutionalized, hospitalized, suffering from some
health condition that prevented them from traveling
to the data collection site, or who had some cognitive
impairment indicated by the FHS team of health
professionals that prevented them from answering
the survey questionnaire. The older adults chosen for the study received an
invitation at their homes, delivered by the Community
Health Agents (CHAs) linked to each FHS team. In the
invitations there was information about the research,
date, time, conditions for attending the FHUs, and the
location chosen for the data collection. If the selected
participant refused to take part, the researchers
chose to invite the next older adult on the list of those
registered with the respective FHS team. If the older
adult was not at home when the CHA visited, this
health professional returned later to try to contact
them. In both cases – refusal and absence – only one
replacement attempt was made. If unsuccessful, we
considered this as a loss of participant at the time of
the data collection. The data collection was carried out by a trained
and standardized multi-professional team, formed
of researchers and graduate students from the
health area, between February of 2017 and August
of 2018. Specific scales were applied to investigate
the main variables of interest (FI and malnutrition), as well as a structured questionnaire with
questions elaborated by the researchers,
which was used to collect the other
information: demographic, social, lifestyle,
health condition, anthropometric, and food
consumption. We evaluated malnutrition/risk of
malnutrition using the Mini Nutritional
Assessment (MNA) (23–25). This instrument
was translated, adapted, and validated for
the Brazilian population and can be used in
older adults in various settings (community,
hospital, and institutional) (26). The MNA
enables a multidimensional analysis of the
older adult, based on a global assessment (life
conditions, use of pharmaceuticals, mobility,
and mental disorders), dietary aspects,
anthropometric indicators, self-perceptions
about health, and NS (23–25). The tool has
high sensitivity and specificity in identifying
nutritional outcomes, as well as a good
correlation with the body mass index (BMI).
After the application of the 18 questions of
the MNA, a score is generated that enables
the older adult’s NS to be classified into one
of three categories: malnutrition (<17 points),
risk of malnutrition (≥17 to ≤23.5 points), or
normal NS (≥24 points) (25,27). We assessed FI using the Brazilian Food
Insecurity Scale (EBIA), a tool that has been
widely used since it was translated, adapted,
and validated for application in Brazil (28,29).
The EBIA is a psychometric scale that
analyzes the family/household perception
and experience regarding FI and hunger,
pondering the difficulties in accessing foods
(30). The scale is formed of 14 dichotomous
questions for households with the presence
of someone under 18 years old and eight
questions in the absence of children and
adolescents in the household. For each
question, a positive answer (yes) corresponds
to one point; and each negative answer (no) is
given zero points (31). After applying the EBIA,
and considering the presence or absence of
individuals under 18, the households with
older adults are classified into four groups: food security (FS) (0 points), mild FI (1-3 points
without someone <18 years old; 1-5 points
with someone <18 years old), moderate FI
(4-5 points without someone <18 years old;
6-9 points with someone <18 years old), and
severe FI (6-8 points without someone <18
years old; 10-14 points with someone <18
years old) (30). To characterize the sample, we calculated the absolute
and relative frequencies of the categorical variables.
We also conducted a bivariate analysis that included
the chi-squared test, considering the associations
between NS (categorized as normal and malnutrition/
risk), FI situation (grouped into FS and FI), and the
covariables. In addition, we ran a binary logistic regression, with
hierarchized modeling, to calculate the crude and
adjusted odds ratios (ORs) and their respective 95%
confidence intervals (CI95%). At this point in the
analysis, FI was presented in three categories: 1) FS,
2) mild FI, and 3) moderate/severe FI. The inclusion of
the independent variables in the models considered
those with p<0.20 in the bivariate analysis, assuming
malnutrition as an output. Model I included only FI;
II added the demographic and social variables; III
included lifestyle and health conditions; and model IV
(the final one) inserted the anthropometric and food
consumption variables. We made an adjustment for
sex and age and for all the analyses we used α = 0.05
to determine the statistical significance. We used
the Statistical Package for the Social Sciences (SPSS,
Chicago, IL, USA), version 20.0, in the analyses. The study participants were informed about the
objectives and procedures of the research they formed
part of. The adhesion of the older adults was voluntary
and dependent on their signature or fingerprint
on the Free and Informed Consent Form (FICF). In
addition, the study was approved by the Research
Ethics Committee of the São Francisco Faculty of
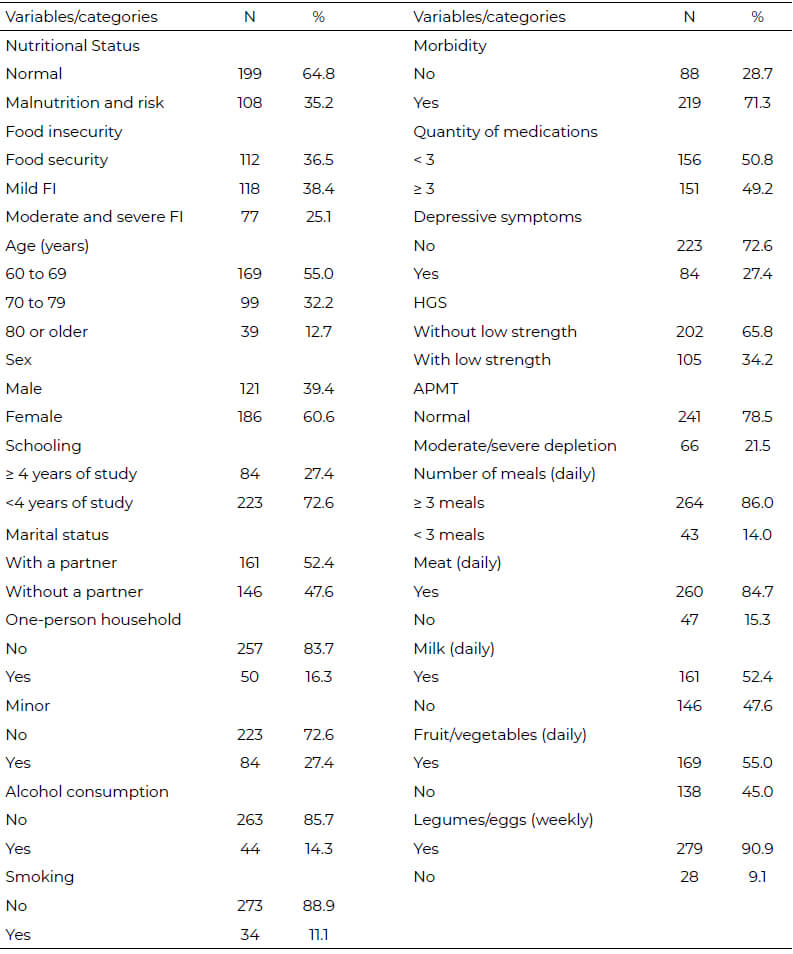
Barreiras (FASB), under case n. 1,447,361/2016. In this study, we evaluated 307 older adults (13.7%
losses), 60.6% of whom were female, with a mean age
of 70.4 (±7.5 years). The prevalence of malnutrition/
risk of malnutrition was 35.2% (3.3% malnutrition and 31.9% risk of malnutrition) and that of FI was 63.5% in
the households with older adults (38.4% mild FI and
25.1% moderate/severe FI) (Table 1). Other characteristics of the sample show that 55.0% of the older adults were aged between 60 and 69
and 72.6% had fewer than four years of study.
A small portion of the older adults lived alone
(16.3%), smoked (11.1%), or consumed some
type of alcoholic drink (14.3%). The presence of at least one morbidity was found in 71.3% of
the older adults and 27.4% of the population
studied presented depressive symptoms.
The results for the anthropometric variables
indicated 21.5% moderate/severe muscle
depletion (APMT) and 34.2% low strength
(HGS). Regarding food consumption, most
of the older adults (86.0%) had three or more
meals a day and frequently consumed meat
(84.7%) and legumes/eggs (90.9%). However,
an important portion did not frequently
consume fruit/vegetables (45.0%) or milk/
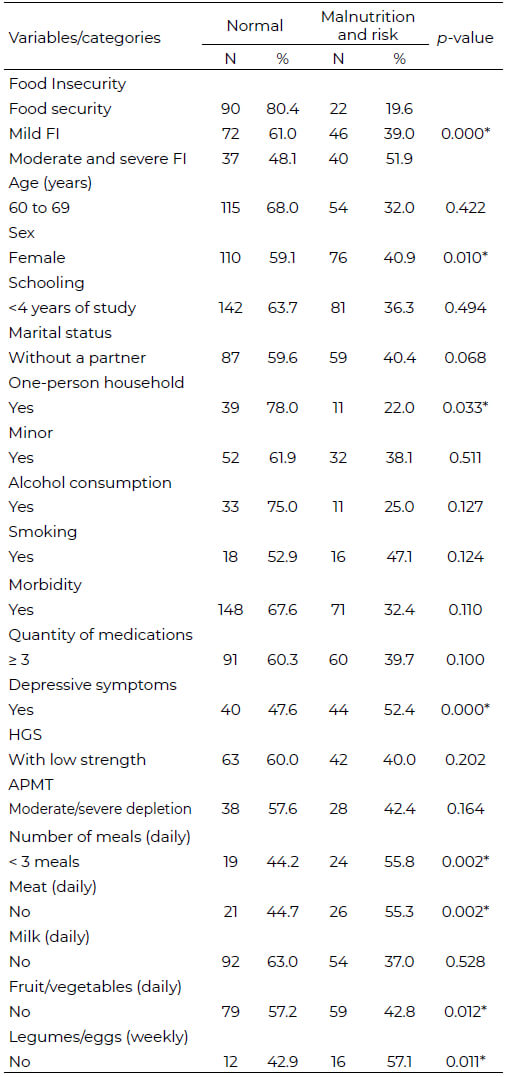
derivatives (47.6%) (Table 1). In the bivariate analysis of the association
between NS and the other variables of the
study, we observed an association between
malnutrition/risk of malnutrition and FI,
sex, one-person households, depressive
symptoms, number of meals, as well as the
dietary consumption variables meat, fruit/
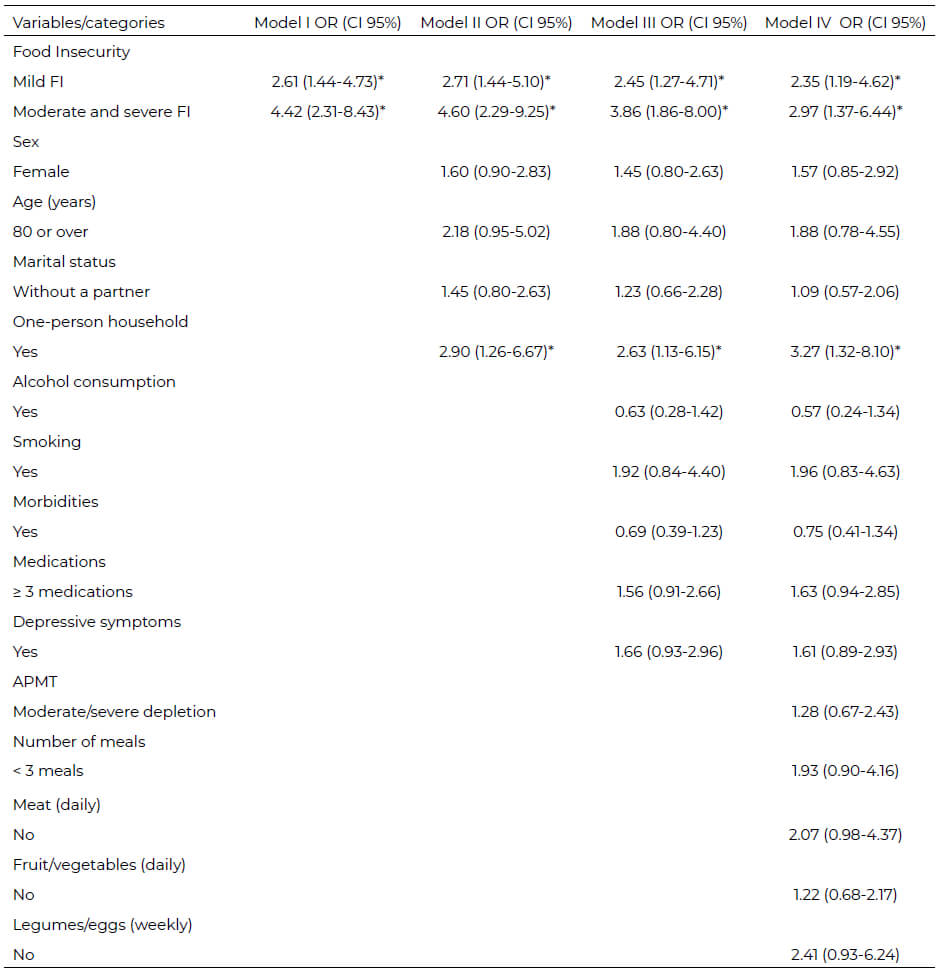
vegetables, and legumes/eggs (Table 2). Table 3 presents the results of the binary
logistic regression, considering the
association between malnutrition/risk of
malnutrition and FI, adjusted by the other
variables present in the hierarchized model.
Model I only considered the association with
FI. The demographic and social variables were
inserted into model II: sex, age, marital status,
and one-person household. In model III we
added the lifestyle (alcohol consumption and
smoking) and health condition (morbidities,
medication, and depressive symptoms)
variables. In the final model (model IV),
after adjusting other variables, we inserted
the anthropometric (APMT) and dietary
consumption (number of meals, meat, fruit/
vegetables, and legumes/eggs) variables.
There was a statistically significant association
between malnutrition and FI from model I up
to the final model, with mild FI presenting
an OR of 2.35 (CI95% 1.19-4.62) and moderate
and severe FI presenting an OR of 2.97 (CI95%
1.37-6.44). The final model fit was observed
through the value obtained in the Hosmer
Lemeshow test (p = 0.601). It was possible to observe that malnutrition/risk of
malnutrition is associated with FI in households of older adults registered with the FHS in a
municipality of the Northeast region of Brazil.
The situation of moderate/severe FI stands
out, which, after adjustments, increased the chance of the older adults developing
malnutrition/risk of malnutrition by 2.97
times, compared with those households living
in FS conditions. These results include FI,
with all of its conceptual complexity, among
the factors that determine malnutrition in
community-dwelling older adults. We also
identified high prevalences of malnutrition/
risk of malnutrition and of FI. In addition,
we observed other factors associated with
the study outcome that explain the multicausal
determination of malnutrition: being
a woman, living alone, presenting depressive
symptoms, having fewer than three meals
a day, and not frequently consuming meat,
fruit/vegetables, or legumes/eggs. A systematic review carried out by Pereira
et al. (7) regarding FI and NS identified
that FI is related with malnutrition/risk of
malnutrition, especially severe FI. In more
severe FI situations, even with the creation
of strategies for them to access foods, older
adults present a reduction in the quantity and
quality of foods consumed, and a consequent
deterioration in NS, with unintentional
weight loss (7,10). Studies conducted in other countries
have also found similar results. Research
conducted in Greece with communitydwelling
older adults who attended
recreation centers found that FI increased
the chance of the participants presenting
the risk of malnutrition by 2.63 times (9). In
Portugal, community-dwelling older adults
in a FI situation presented 72% more chance
of developing malnutrition (36). In another
study conducted using older Turkish adults on
a low income, the presence of FI significantly
increased the risk of malnutrition (6). High prevalences of malnutrition and FI have
been found in other studies of communitydwelling
older adults. In Brazil, research that
used the MNA on older adults cared for by
the FHS indicated that malnutrition/risk of
malnutrition varied from 24.1% to 46.5% (37,38).
A systematic review with a meta-analysis that
evaluated 58 studies of community-dwelling
older adults indicated a 26.5% (CI95% 22.4-
32.7) prevalence of malnutrition/risk of
malnutrition (39). The prevalence of FI in studies of Brazilian community-dwelling older adults
varied from 21.8% to 52% (40,41). One recent study
conducted in South America (older Colombian adults)
observed 55% FI. In an analysis of 22 studies, Pereira
et al. (7) showed the prevalence ranged from 1.7% in
older North American adults to 76.3% in older Greek
adults. That is, given a heterogeneous aging process
between countries and social classes, being an older
adult is a risk factor for FI and malnutrition, especially
among community dwellers. Community-dwelling older adults experiencing FI
who are treated in social programs such as the FHS
generally present a social, health, and dietary situation
that can cause a greater chance of them developing
malnutrition. Social vulnerability is perceived that
primarily hinders access to and the stability of an
adequate and healthy diet, in the face of so many other
priorities (36,38,43). In addition, there is a combination
of aspects related with the health condition of older
adults, such as the physiological repercussions of
aging itself, as well as those derived from pathological
processes, which influence the older adult’s diet
and can affect their NS (44). Moreover, older adults
experiencing FI present an unstable and insufficient
dietary pattern that may not meet the nutritional
recommendations (7,45). To mitigate this situation,
many older adults resort to social programs, such as
income transfer programs, community restaurants,
food banks, and meal distributions (41,46). In spite of the effort employed in all the stages of
the research, the study presents some limitations.
One of these relates to the use of the EBIA, which
places more emphasis on assessing aspects related
to the access to foods dimension; as well as using
households/families with older adults as an analysis
unit, and not necessarily the older individual (30).
Nonetheless, the scales or questionnaires based on
the family experience of FI and hunger are the most
widely used instruments for assessing the topic and
focus on the acquisition of foods, due to the robust
scientific evidence, which considers economic aspects
to be the most relevant in determining FI (47). On the
other hand, we highlight the strengths of the study:
1) it focuses on community-dwelling older adults who
use the FHS and PHC; 2) as far as we know, it is the
first study on the topic in Brazil, conducted using a
representative sample of older adults from the FHS;
3) it uses the MNA to assess malnutrition, which is
a multidimensional instrument that is widely used
in research and in nutritional assistance, and which
considers the specificities of aging (25). There is an association between food insecurity and
malnutrition/risk of malnutrition in older adults
attended to under the Family Health Strategy, with
moderate/severe FI standing out. In addition, this study
indicates that households with older adults registered
with the FHS present high prevalences of both food
insecurity and malnutrition, possibly due to the
vulnerabilities present in the individual and collective
context of these individuals. Finally, the results include
FI as one of the determinants of malnutrition among
community-dwelling older adults, together with
other social, health, and nutritional aspects, which are
already well-established in the literature. We are grateful to all the older adults who participated
in the research; to the professionals of the Family
Health and Primary Care teams of the municipality
of Barreiras (BA), who enabled the data collection; as
well as to the students and professors who took part
in the working group of the research project. The authors declare they have no conflict of interests. Funding: Not applicable. Recibido: 22/08/2022Inclusion and exclusion criteria
Data collection
Outcome: malnutrition/risk of malnutrition
Exposure variable: food insecurity
Covariables
Statistical analysis
Ethical aspects
Results
APMT: adductor pollicis muscle thickness; OR: odds ratio; IC: 95% Confidence Interval.Discussion
Conclusions
Acknowledgements
Conflict of Interest
REFERENCIAS
Aceptado: 24/11/2022